The Joints of Hubert von Luschka
A Unique Chiropractic Perspective
The spot where two bones come together is called a joint. Some joints do not allow for much motion, like the joints between the various bones of the skull. Other joints allow for smooth movement between the adjacent bones. These joints are called synovial joints.
The spinal column is divided into three distinct regions:
-
- Lumbar (low back)
- Thoracic (middle back)
- Cervical (neck)
The spinal column displays great mobility. This allows humans to bend down and touch their toes and to rotate their head over their shoulder to check for traffic while driving. These magnitudes of motion are largely attributed to the spinal synovial joints.
The three regions of the spinal column show large differences in their mobility (1, 2, 3). The least moveable region is the thoracic spine. This is because the ribs attach to the thoracic spine vertebrae, come around to the front of the body and attach to the sternum (breast bone).
The mobility of the lumbar spine region is greater than that of the thoracic spine, but not as large as the cervical spine. The cervical spine has the greatest mobility, attributable to a special reason that is discussed below.
A primary concern for chiropractors is the mobility between the synovial joints of the spinal column. Chiropractors assess spinal joint mobility using a variety of investigational tools (observation, imaging, palpation, etc.). Once the level and direction of the reduced motion is identified, chiropractors deliver a force to the joint to improve the direction and magnitude of its motion (4). Chiropractors call this specifically delivered force an adjustment (a specific line-of-drive manipulation).
Improving synovial joint mobility has a number of physiological influences, the best understood of which is the closure of the pain gate (4, 5, 6). The bottom line is that this means that chiropractic spinal adjusting is quite effective in the management of spinal pain syndromes (4, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16).
Synovial joints have these defining characteristics:
-
- Articular hyaline cartilage
- An articular capsule that creates a joint cavity
- The articular capsule is neurologically innervated with nociceptors (pain afferents), mechanoreceptors (for proprioception), and with sympathetic nerves
- The joint cavity is filled with synovial fluid
The primary synovial joints of the spine are located in the posterior (back) half of the vertebrae, behind the exiting nerve root. These spinal synovial joints are known as the facet joints or the zygapophysial joints. Typically, each spinal vertebrae has four facet synovial joints:
-
- Two on the top of the vertebrae (left and right)
- Two on the bottom of the vertebrae (left and right)
Uniquely, importantly, and the main topic of this paper, the cervical spine has four additional synovial joints per spinal vertebrae level (two on the top, left and right, and two on the bottom, left and right).
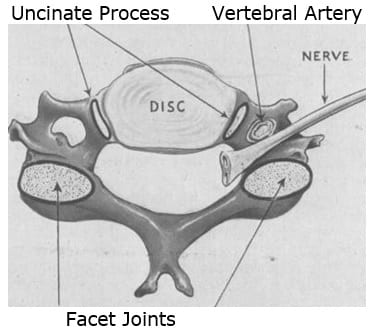
In the graphic above, the view is axial, looking from above at the superior (top) margin of a cervical vertebrae. The facet joints, behind the nerve root, are clearly noted. Notice the structures labeled “Uncinate Process,” lateral to the intervertebral disc. The uncinate processes are a component of a synovial joint known as the Uncovertebral Joints.
The uncinate processes and uncovertebral joints were first described in 1834, and later described in detail by German anatomist Hubert von Luschka in 1858. Hence, these joints are often referred to as the joints of von Luschka.
Hubert von Luschka was a German anatomist. He was born is 1820. He was appointed a full professor of anatomy in 1855 at the University of Tubingen. He gained a noble title and began using von in his name in 1865.
The joints of von Luschka are located in the cervical region of the spinal column between C3 through C7, in all specimens. In some individuals, these joints are also located in the upper thoracic spine region. These joints allow for cervical spinal flexion and extension while limiting cervical spinal lateral flexion.
In 1958, the Journal of the American Medical Association published a study titled (17):
Whiplash Injuries:
Neurophysiological Basis for Pain
and Methods Used for Rehabilitation
This study appeared literally 100 years after the original descriptions of the joints of von Luschka by Herbert von Luschka. The author, Emil Seletz, MD, (b. 1907; d. 1999) was a neurosurgeon in Beverly Hills, California. His publications indicate that Dr. Seletz worked at the Los Angeles General Hospital, and he was faculty at the University of California, Los Angeles, Medical School. His is internet biography indicates he was chief of neurosurgery at Cedar’s Hospital (now called Cedars-Sinai Medical Hospital) in Los Angeles, and Professor of Neurological Surgery at the University of Southern California School of Medicine.
In this article, Dr. Seletz profiles whiplash injuries, and it includes a discussion pertaining to the uncinate processes and the joints of von Luschka. The importance of this discussion lies in that these joints limit lateral flexion. Whiplash mechanisms that involve lateral flexion stress, or any mechanism where the patient’s head/neck are in rotation at the time of impact, have increased potential to cause injury to the uncinate processes and/or the joints of von Luschka.
In this article, Dr. Seletz makes these points:
-
- Cervical discs degenerate following whiplash trauma.
- The cervical vertebrae also contain “special synovial joints,” the lateral body joints of von Luschka, first described in 1858.
- In whiplash injury, the joints of von Luschka play a very significant clinical role.
- “With degenerative thinning of the disk after trauma, the processes of the lateral joints [uncinate] are gradually forced outward and laterally, resulting in osteophyte formation.”
- Lateral spurs from the joints of von Luschka compress the nerve root and can encroach on the vertebral artery and the vertebral nerve (sympathetic) within the foramen transversarium.
- The joints of von Luschka are synovial joints with a cartilage cap.
- “These spurs project even more, since the osteophytes are capped with cartilage and are considerably larger than is revealed by the roentgenogram.”
The following year, 1959, Edward Compere, MD, and colleagues, published a study in the journal Orthopedics, titled (18):
The Luschka Joints; Their Anatomy, Physiology and Pathology
Dr. Compare was an orthopedic surgeon, and Professor of Bone and Joint Surgery at Northwestern University (Chicago). In this publication, the authors note that the joints of von Luschka demonstrated all of the elements of a true joint in microscopic sections. This adds support to the understanding that these joints are synovial.
In 1978, Ruth Jackson, MD, published the fourth edition of her book, The Cervical Syndrome (19). Ruth Jackson, MD (1902-1994), was the world’s first female admitted into the American Academy of Orthopedic Surgeons (1937). She began her orthopedic private practice in Dallas in 1932. From 1936 to 1941, Dr. Jackson was Chief of Orthopaedics at Parkland Hospital in Fairmont, Texas. In 1945, she had her own private clinic built in Dallas. In 1956 she published the first edition of her acclaimed, authoritative book, The Cervical Syndrome. Dr. Jackson retired from clinical practice in 1989 at the age of 87 years.
In her book, Dr. Jackson has a section pertaining to the joints of von Luschka, beginning with their injury vulnerability to lateral-flexion mechanical stress. She notes:
-
- The joints of von Luschka “are covered with articular hyaline cartilage, as are all other articulating surfaces.”
- “These articulating surfaces were described as true joints with capsules and synovial linings by von Luschka in 1858.”
- “The adjacent surfaces at the sides of the bodies of the vertebrae are plated with articular cartilage,” and “capsular ligaments are present.”
- “There is a definite space between the adjacent articular surfaces.”
- “These articulations do satisfy the standard definition of synovial joints.”
- “Osteophytic formations do occur at the margins of the articulations which is characteristic of synovial joints.”
Most importantly, Dr. Jackson demonstrates that the injection of radiopaque dye into the joints of von Luschka shows that the material remains confines, as in being held by a capsule.
In 2009, Jean-Michel Brismée, ScD, and colleagues from the School of Allied Health Sciences, Texas Tech University Health Sciences Center, published a study in the journal Spine titled (20):
Immunohistochemical and Histological Study
of Human Uncovertebral Joints
The authors of this study claim that no research had investigated the presence of pain generating neurotransmitters within the uncovertebral cartilaginous and capsular tissue. Consequently, this study investigated the anatomy and innervation of the uncovertebral joints to determine if it is synovial in nature and if it was capable of generating pain.
The study used two unembalmed fresh male human cadavers with a mean age of 83 years. Tissue from the uncovertebral capsule and cartilage was harvested from each uncovertebral surface from C2-C3 to C6-C7.
The findings included the identification of chondrocytes and synoviocytes in the capsular tissue of each uncovertebral joints. This indicates that the uncinate joints have articular hyaline cartilage and a synovial capsule. This indicates that the uncovertebral joint is “synovial in nature.”
The authors also assessed the harvested uncinate capsular tissue for neurofilaments using immunohistochemistry. The immunoreactivity findings indicated that the uncinate capsules also have the presence of both the somatic and autonomic nerve fibers. “These findings suggest that the uncovertebral joints are potential pain generators in the cervical spine.”
The authors noted that these capsular and synovial tissue nerve fibers lead to pain perception and reflexive responses associated with synovial pathology. They make these comments:
Biomechanically, the “uncovertebral joint is a major contributor to coupled motion at the lower cervical spinal segments and serves as a controlling factor of overall cervical segmental motion.”
“A synovial or diarthrodial joint must exhibit a joint capsule, a synovial membrane, synovial fluid, and articular cartilage.” “Our present findings support the notion that the uncovertebral complex includes a synovial joint.”
Disc degeneration always influences the uncinate joints, their biomechanics and their degenerative potential.
Degenerative changes in the uncinate joints may translate into osteophytic projections that can compress adjacent cervical segmental nerves as they course through the intervertebral foramen or may cause cervical myelopathy.
“Due to the close proximity of the uncinate process to the vertebral artery degenerative changes in the uncovertebral joint have been clinically related to vertebral artery compression, ultimately lending to the onset and severity of clinical vertebrobasilar insufficiency.”
The authors conclude that there should be no controversy with regard to the anatomic and histological makeup of the uncovertebral joints. They are synovial joints that possess a joint cavity that is lined with a synovial membrane secretes synovial fluid. They imply that authors who claim otherwise are incorrect.
In 2014, Jeffery Hartman, MD, from the College of Medicine, University of Saskatchewan, Canada, published a “Comprehensive Review” titled (21):
Anatomy and Clinical Significance of
the Uncinate Process and Uncovertebral Joint
In this “comprehensive review,” Dr. Hartman cites 74 references of the literature, making this review the most extensive published review on this topic to date.
Dr. Hartman notes that the uncinate process and its associated uncovertebral articulation are unique to the cervical spine. They are rudimentary at birth and develop and evolve with age. They are consistently found on the posterolateral aspect of the superior end plate of the third to seventh cervical vertebrae. However, in some individuals, they extend as low as to the T2 level.
The uncinate processes guide the motions of the cervical spine. They also provide important lateral stability for the cervical spinal motions. The uncinate processes function to limit lateral flexion. Dr. Hartman states:
“Although often overlooked due to their relatively small size the uncovertebral articulation has been shown to contribute to the stability of the cervical spine.”
“The uncovertebral articulation contributes to the spinal motion segments mobility and stability as well as functions to protect the intervertebral foramen contents from herniated disc material.” [see Graphic 1]
“The spinal segments’ mobility throughout flexion, extension, lateral flexion, and rotation is influenced by the structure of the uncinate processes and their articulation with the vertebra above.”
Motion in the coronal plane that occurs during lateral flexion is coupled with axial rotation. The uncovertebral articulation is a significant contributor to this coupled motion.
“In addition to influencing the mobility of the spinal segments the uncinate processes provide stability.”
As noted above, the location of the uncinate processes makes them a barrier to lateral and posterior-lateral herniations of the cervical intervertebral disc. To support this, Dr. Hartman references a 2003 study from the journal Spine (22). It was a study of 200 patients with myelopathy or radiculopathy secondary to cervical intervertebral disc herniation. One hundred and ninety-eight (198) of the herniations were median or paramedian; only two were lateral herniations. Both of the two lateral herniations occurred at C7-T1, where the uncovertebral articulation is rudimentary or absent. The authors concluded:
“It was concluded that the uncovertebral articulations prevent lateral herniations.”
Lateral intervertebral disc herniations at C7-T1 are more common than other cervical segments because of the “lack of barrier provided by the uncinate processes.”
The uncinate processes and joints are especially vulnerable to side-impact or rotation-type neck trauma. These articulations are commonly disrupted in head and neck injuries. Uncovertebral cleft hematomas are commonly seen in victims of traffic accidents. Following such trauma, the cervical intervertebral disc degenerates at an accelerated rate. This disc degeneration deflects more weight-bearing responsibility to the uncinate processes, accelerating spondylotic changes of these joints.
The uncinate processes bear the load of the vertebra above. With age and/or injury, the intervertebral disc dehydrates and thins, leading to an increased load being supported by the uncinate processes. With this degeneration, the uncinate processes and uncovertebral articulations may compress the spinal nerve root and vertebral artery. Dr. Hartman makes these statements:
“Dehydration and narrowing of the cervical intervertebral discs begin to occur in the fourth and fifth decades of life.”
With age, the “uncinate process develops osteophytic lipping where the tip turns laterally.”
“With narrowing of the intervertebral discs, the uncinate processes bear a greater load to support the weight of the head.”
“The vertebra above comes to rest on the uncinate processes below which results in remodeling to the flattened and laterally directed configuration.”
“The uncovertebral articulations are common sites for osteoarthritic changes.”
“These changes are believed to be related to the dehydration and shrinkage of the intervertebral disc which leads to increased load and contact between the vertebra above and the uncinate processes below.”
“The osteophytic spurring from the uncinate processes project laterally and thus can impinge on anatomical structures within the vicinity, including the spinal nerve root, vertebral artery, radicular (medullary) artery, cervical spinal cord, and cervical sympathetic trunk.”
“The reduced blood flow through the radicular artery from external compression is a contributing factor to the development of cervical spondylotic myelopathy.”
“Osteophytes that arise from the posterior aspect of the uncinate process project into the intervertebral foramen and encroach on its contents.”
When the vertebral artery is compressed by osteophytes they are “more likely to be derived from the uncinate process than from the zygapophysial joints.”
“In cervical spondylosis, the uncovertebral osteophytes are the most common cause of nerve root compression.”
The degenerative changes described narrow the intervertebral foramen, increasing the incidence of nerve root irritation and/or compression:
“The clinical picture resulting from cervical nerve root compression is one of pain, paraesthesia, diminished sensation to pinprick, diminished reflexes, muscle weakness, and, rarely, muscle wasting in the neck and ipsilateral upper extremity.”
Dr. Hartman also notes that when there is an acute injury to the uncinate process, the synovial joint becomes inflamed and edematous. The resulting pain and spasm may precipitate an acute cervical torticollis.
Summary and Concluding Remarks
Ongoing evidence for 150 years continues to support the anatomy that the uncinate is a synovial joint with articular hyaline cartilage, a joint capsule, a synovial bag that produces synovial fluid, an is neurologically innervated and thus capable of producing pain. Like all other synovial joints, these joints of von Luschka may develop mechanical problems, open the pain gate, and cause neck pain.
Many chiropractors contend that uncinate joint mechanical problems (chiropractic subluxation) can be improved with an appropriately delivered spinal adjustment. The uncinate joint subluxation is distinct from the facet joint subluxation. The adjustment of the uncinate joint subluxation is also distinct from the facet joint subluxation adjustment. Traditionally, the adjustment of facet joint subluxation is delivered at the back of the neck, often the contact is made with the fingertip or with an approved mechanical device. In contrast, the uncinate joint adjustment is often delivered to the front of the neck, and frequently the contact is made with the thumb or, again, with an approved mechanical device. The skills to successfully deliver these maneuvers is emphasized in chiropractic education.
Lastly, with advancing degenerative changes to the uncinate processes, there may be irritation of the cervical nerve roots or possibly to the neurological controls of the vertebral artery. Ideally, carefully delivered chiropractic adjusting will improve biomechanical function and reduce the adverseness of such irritations.
REFERENCES
- Cailliet R; Low Back Pain Syndrome; 4th edition; FA Davis Company; 1981.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine; Second Edition; Lippincott; 1990.
- Kapandji AI; The Physiology of the Joints: The Spinal Column, Pelvic Girdle and Head; Seventh Edition; Handspring Publishing; 2019.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low Back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-540.
- Melzack R, Wall P; Pain mechanisms: a new theory; Science; November 19, 1965;150(3699); pp. 971-979.
- Dickenson AH; Gate Control Theory of Pain Stands the Test of Time; British Journal of Anaesthesia; June 2002; Vol. 88; No. 6; pp. 755-757.
- Giles LGF; Muller R; Chronic Spinal Pain: A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation; Spine July 15, 2003; Vol. 28; No. 14; pp. 1490-1502.
- Muller R, Giles LGF; Long-Term Follow-up of a Randomized Clinical Trial Assessing the Efficacy of Medication, Acupuncture, and Spinal Manipulation for Chronic Mechanical Spinal Pain Syndromes; Journal of Manipulative and Physiological Therapeutics; January 2005; Vol. 28; No. 1; pp. 3-11.
- Adams J, Peng W, Cramer H, Sundberg T, Moore C; The Prevalence, Patterns, and Predictors of Chiropractic Use Among US Adults; Results From the 2012 National Health Interview Survey; Spine; December 1, 2017; Vol. 42; No. 23; pp. 1810–1816.
- Meade TW, Dyer S, Browne W, Townsend J, Frank OA; Low back pain of mechanical origin: Randomized comparison of chiropractic and hospital outpatient treatment; British Medical Journal; Vol. 300; June 2, 1990; pp. 1431-7.
- Woodward MN, Cook JCH, Gargan MF, Bannister GC; Chiropractic treatment of chronic ‘whiplash’ injuries; Injury; November 1996; Vol. 27; No. 9; pp. 643-645.
- Khan S, Cook J, Gargan M, Bannister G; A symptomatic classification of whiplash injury and the implications for treatment; The Journal of Orthopaedic Medicine; Vol. 21; No. 1; 1999; pp. 22-25.
- Hoving JC, Koes BW, de Vet HCW, van der Windt DAWM, Assendelft WJJ, Mameren H, Devillé WLJM; Manual Therapy, Physical Therapy, or Continued Care by a General Practitioner for Patients with Neck Pain; A Randomized Controlled Trial; Annals of Internal Medicine; May 21, 2002; Vol. 136; No. 10; pp. 713-722.
- Fischgrund JS; Neck Pain, Monograph 27, American Academy of Orthopaedic Surgeons; 2004.
- César Fernández-de-las-Peñas; J. Fernández-Carnero; L. Palomeque del Cerro; Manipulative Treatment vs. Conventional Physiotherapy Treatment in Whiplash Injury: A Randomized Controlled Trial; Journal of Whiplash & Related Disorders; 2004; Vol. 3; No. 2.
- Langenfeld A, Humphreys K, Swanenburg J, Cynthia K. Peterson CK; Prognostic Factors for Recurrences in Neck Pain Patients Up to 1 Year After Chiropractic Care; Journal of Manipulative and Physiological Therapeutics; September 2015; Vol. 38; No. 7; pp. 458-464.
- Seletz E; Whiplash Injuries: Neurophysiological Basis for Pain and Methods Used for Rehabilitation; Journal of the American Medical Association; November 29, 1958; Vol. 168; No. 13; pp. 1750–1755.
- Compere EL; The Luschka Joints; Their Anatomy, Physiology and Pathology; Orthopedics; May 1959; Vol. 1; pp. 159-167.
- Jackson R; The Cervical Syndrome; fourth edition; Charles Thomas; 1978.
- Brismée JM, Sizer PS, Dedrick GS, Sawyer BG, Smith MP; Immunohistochemical and Histological Study of Human Uncovertebral Joints; Spine; May 20, 2009; Vol. 34; No. 12; pp 1257-1263.
- Hartman J; Anatomy and Clinical Significance of the Uncinate Process and Uncovertebral Joint: A Comprehensive Review; Clinical Anatomy; April 2014; Vol. 27; No. 3; pp. 431–440.
- Yamazaki S, Kokubun S, Ishii Y, Tanaka Y. 2003. Courses of cervical disc herniation causing myelopathy or radiculopathy: An analysis based on computed tomographic discograms; Spine; June 1, 2003; Vol. 28; No. 11; pp. 1171–1175.
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

