Why Do Patients Go To Chiropractors?
Inflammation
In her books, Epigenetics Revolution (2013) and Junk DNA (2017) geneticist Nessa Carey explains that the driving force in human evolution and in human biology is procreation; living long enough to make babies and pass our genes on to future generations (1, 2). At the center of the human opportunity to procreate is a biological process that increases individual survivability and hence the ability of that individual to procreate: inflammation.
Dale Bredesen, MD, is unique. He is a neurologist from the Department of Neurology, University of California, Los Angeles, CA, USA (UCLA). He is conducting ongoing clinical trials pertaining to the reversal of Alzheimer’s disease, including in individuals that are genetically homozygous (they have two alleles) for the most prominent risk factor for the disease (3, 4, 5).
A distinction between Dr. Bredesen and other researchers and clinicians in this field is that Bredesen does not believe that Alzheimer’s disease is caused by the accumulation of the fibrotic proteins amyloid and/or tau. In contrast, he proposes that amyloid and/or tau proteins exist in response to chronic inflammation of the brain. He states (5):
“When our ancestors became bipedal, descending from the trees and walking the savanna, inflammation was actually an advantage.”
“Inflammation is part of the reaction by the immune system to foreign invaders, allowing our ancestors to survive stepping on dung, puncturing their feet, eating raw meat filled with pathogens, and sustaining wounds during hunts as well as while fighting with each other.”
“In all of these situations, mounting a robust inflammatory response protects against life-threatening infection.”
“As we age, however, inflammation promotes cardiovascular disease, arthritis, and other woes—including Alzheimer’s disease.”
“This trade-off is called antagonistic pleiotropy, in which a genetic alteration enhances fitness early in life at the expense of longevity.”
The “other woes” caused by the inflammation mentioned by Dr. Bredesen includes fibrotic changes around and in joints, leading to joint dysfunction. Common terminology in the chiropractic profession for these articular fibrotic changes include “the fibrosis of repair,” “periarticular fibrosis,” “intra-articular fibrosis,” “intra-articular adhesions,” “granulation tissue,” “scar,” etc. These inflammatory driven fibrotic changes may protect an individual from the spread (and death from) infection, but they also cause articular movement or positional dysfunctions called the “subluxation.” (6)
The June 2015 issue of the journal Scientific American has an article by physician Wajahat Z. Mehal, MD, from the Department of Veterans Affairs Medical Center in Connecticut, and Yale University, titled (7):
Cells on Fire
In this article, Dr. Mehal notes that inflammation is set in motion by the cells of the immune system, and that it is helpful because it kills pathogens and blocks their spread in the body. The inflammatory cascade weakens and immobilizes adverse microbes that otherwise make humans sick and increases mortality, thus reducing procreation.
The same inflammatory cascade can occur when no microbes exist, triggered as a consequence of tissue injury and/or excessive tissue stress. This inflammatory response can, in-and-of-itself, become chronic and cause additional tissue damage. In other words, as much as acute inflammation can be beneficial (containing and/or killing pathogens), chronic inflammation can be deleterious, serving no useful purpose.This inflammatory response, with no associated pathogens, often leads to chronic joint motion problems.
Historically, these concepts of inflammation (from any cause) leading to “walling-off,” repair and fibrosis have been well documented in pathology books, often being given an entire chapter of emphasis. Examples include:
In 1952, William Boyd, MD, Professor Emeritus of Pathology at the University of Toronto, published in his reference text (8):
PATHOLOGY
Structure and Function in Disease
“The inflammatory reaction tends to prevent the dissemination of infection. Speaking generally, the more intense the reaction, the more likely the infection to be localized.”
In 1970, the eighth edition of Dr. Boyd’s PATHOLOGY text is published (9): In chapter 4, titled “Inflammation and Repair,” Dr. Boyd states:
“Inflammation is the most common, the most carefully studied, and the most important of the changes that the body undergoes as the result of disease.”
Dr. Boyd notes that in chronic inflammation, the “only cells that proliferate are the fibroblasts.” Consequently, the chronic inflammatory response is considered to be a “fibroblast reaction,” or “fibrosis.” The lesion of chronic inflammation becomes more and more fibrous as the collagen is laid down. The resulting fibrosis is much more marked than in acute inflammation situations. Also, the “newly-formed fibrous tissue invariably contracts as it becomes older.”
In 1976, physicians WAD Anderson, MD, and Thomas Scotti, MD, published the ninth edition of their book titled (10):
Synopsis of Pathology
Drs. Anderson and Scotti were Professors of Pathology at the University of Miami School of Medicine. Similar to Boyd, they titled chapter 3 of their text “Inflammation and Repair,” in which they state:
“Inflammation is the most common and fundamental pathological reaction.”
The agents leading to inflammation include “microbial, immunologic, physical, chemical, or traumatic.”
“Chronic inflammation is a process that is prolonged, and proliferation (especially in connective tissues) forms a prominent feature.”
“The proliferative activity, leading to the production of abundant scar tissue, may in itself be distinctly harmful.”
“The final healed state is achieved by development of a connective tissue scar.”
An important premise from Drs. Anderson and Scotti is that in chronic inflammation, “abundant” scar tissue may form, and this connective tissue scar may “itself be distinctly harmful.” Connective tissue is the tissues of joints, and the harm to the joints is reduced movement.
In 1979, Harvard Medical School professors Stanley Robbins, MD, and Ramzi Cotran, MD, published the second edition of their book, titled (11):
PATHOLOGIC BASIS OF DISEASE
Similar to Boyd, Anderson and Scotti, Robbins and Cotran also titled chapter three of their text “Inflammation and Repair.” Robbins and Cotran state:
“Inflammation serves to destroy, dilute, or wall-off the injurious agent.”
“Without inflammation, bacterial infections would go unchecked.”
But, “inflammation itself may be potentially harmful.”
Chronic inflammation is “generally of longer duration and is associated histologically with the presence of lymphocytes and macrophages and the proliferation of small blood vessels and fibroblasts.”
Tissues are replaced by “filling the defect with less specialized fibroblastic scar-forming tissue.”
“Reparative efforts may lead to disfiguring scars, fibrous bonds that limit the mobility of joints, or masses of scar tissue that hamper the function of organs.”
It is of particular interest to note that Drs. Robbins and Cotran specifically note that the cascade of inflammation and fibrosis may “limit the mobility of joints.”
In the second edition of their book, Guido Manjo, MD and Isabelle Joris, PhD, talk extensively about inflammation and fibrosis, stating (12):
Cells, Tissues, and Disease
Principles of General Pathology
“Inflammation is one of the basic processes in general pathology.”
“Inflammation is primarily an antibacterial phenomenon.” “Today we know that inflammation is a life-saving reaction, usually against infection.”
The evolutionary significance of inflammation is as a primary antibacterial response. “It is a matter of urgency. The doubling time of common pathogenic bacteria is of the order of 20 minutes.”
“Inflammation is also triggered aseptically by injured tissues.”
“There can be inflammation without infection; remember that inflammation is triggered by products of tissue injury, thus any aseptic injury will trigger inflammation.”
“Because local injury is part of everyday life, inflammation is probably the most common aspect of tissue pathology and has always been perceived as a central issue in the practice of medicine.”
Granulation tissue “is a key component of chronic inflammation.” “Granulation tissue arises from normal connective tissue, but it cannot be mistaken for normal connective tissue.”
“With time, granulation tissue loses most of its cells, the collagen component increases, and the terminal picture blends with that of scar.”
“When fibrosis develops in the course of inflammation it may contribute to the healing process.” “By contrast, an excessive or inappropriate stimulus can produce severe fibrosis and impair function.”
“Why does fibrosis develop? In most cases the beginning clearly involves chronic inflammation. Fibrosis is largely secondary to inflammation.”
Important observation by Drs. Manjo and Joris include:
-
- Injury is part of everyday life
- Inflammation is the body’s response to injury
- Inflammation results in tissue fibrosis
- Inflammation and fibrosis is the most common tissue pathology and “has always been perceived as a central issue in the practice of medicine.”
•••
Orthopedic, clinical management, and physiology texts also discuss inflammation and fibrosis.
In 1982, orthopedic surgeon Sir James Cyriax, MD, published the eighth edition of his book titled (13):
Textbook of Orthopaedic Medicine:
Diagnosis of Soft Tissue Lesions
In this text, Dr. Cyriax notes that harmful infections create tissue destruction, resulting in inflammation. Our body recognizes this inflammation and attempts to “wall off” the infectious pathogens by creating a fibrous response. Cyriax states:
“The excessive reaction of tissues to an injury is conditioned by the overriding needs of a process designed to limit bacterial invasion. If there is to be only one pattern of response, it must be suited to the graver of the two possible traumas. However, elaborate preparation for preventing the spread of bacteria is not only pointless after an aseptic injury, but is so excessive as to prove harmful in itself. The principle on which the treatment of post-traumatic inflammation is based is that the reaction of the body to an injury unaccompanied by infection is always too great.”
In 1983, physicians Steven Roy and Richard Irvin published their book on sports injury titled (14):
Sports Medicine:
Prevention, Evaluation, Management, and Rehabilitation
In this book, Roy and Irvin state:
“It is important to realize that the body’s initial reaction to an injury is similar to its reaction to an infection. The reaction is termed inflammation and may manifest macroscopically (such as after an acute injury) or at a microscopic level, with the latter occurring particularly in chronic overuse conditions.”
In 1986, physician and physiologist, Arthur Guyton, MD, published the seventh edition of his book, titled (15):
Textbook of Medical Physiology
Dr. Guyton states:
“One of the first results of inflammation is to ‘wall off’ the area of injury from the remaining tissues.”
“This walling-off process delays the spread of bacteria or toxic products.”
In 1992, physician I. Kelman Cohen and associates published their book titled Wound Healing, Biochemical & Clinical Aspects (9), in which they state:
“There are two important consequences of being a warm-blooded animal. One is that body fluids make optimal culture media for bacteria. It is to the animal’s advantage, therefore, to heal wounds with alacrity in order to reduce chances of infection.”
“The prompt development of granulation tissue forecasts the repair of the interrupted dermal tissue to produce a scar.” In addition to providing tensile strength, scars are believed to be a barrier to infectious migration.
Motion
Much of life is dependent upon motion and mobility (17).
Historically, human survival is dependent upon external motion to obtain food, shelter, mates, protection, safety, etc. This is true for other animal species as well.
Internal motion is also critically important. Motion of and between the various parts of the body is critical for the internal health of the human, as well as for other animals.
The 202 joints of the human body are designed specifically to allow for motion between our various body parts. They also allow for the human body to move from place to place.
The movement of every joint in the body can be measured, quantified. The optimal movement for every joint in the body has been established. Increases or decreases in measured joint movements are not good. Such changes in joint movement are frequently associated with pain, degenerative joint arthritis, joint dysfunction, and weakness. These joint movement problems can cause impairments and disabilities. In fact, when they are precisely quantified, the results are often used by government agencies, courts, and medical personnel to establish official impairment and disability status of individuals (18).
Joint movement is divided into three categories (19, 20, 21, 22, 23):
-
- Active Motion
- Passive Motion
- Periarticular Paraphysiological Space Motion
Active Motion
Active Motion is the best understood category of joint motion. It is the type of motion joints experience when people move any part of their body. It requires active contraction of our muscles. Active motion is the typical motion joints experience when people engage in the activities of normal life (showering, dressing, preparing meals, driving, working, shopping, etc.), and exercise. With exercise, specific joints can be targeted for motion benefits and therapy.
Yet, it is important to understand that active motion, including specific exercise active motion, only benefits the most narrow range of tissues, and as such the therapeutic benefit of active motion is limited. When a specific joint is moved through the maximum active range of motion, a natural physiological barrier is met, beyond which no additional motion is possible without assistance (below). The important concept is that joints have the ability to move beyond the active range, and this can be done without causing any stress or injury to the joint.
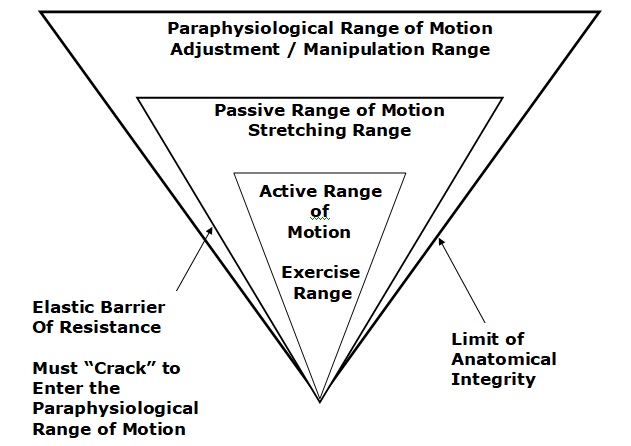
Passive Motion
Passive motion is the passive moving of a joint further than the motion achieved with active motion. Passive motion always affects a greater range of tissue than does active motion. This allows passive motion techniques to better address (treat, manage) tissue fibrosis and joint stiffness.
Accepted and beneficial passive motion applications include stretching, yoga, etc. A variety of health care providers, including chiropractors, are trained and able to isolate specific joints that are lacking optimal motion and to “push” the joint beyond the active range of motion and into the passive range of motion. Again, this is accomplished without any tissue injury.
At the end of the passive range of motion, another “barrier” is encountered. This is called the elastic barrier. Movement beyond the elastic barrier is not only beneficial, it is often critically required. It is also tricky, as noted by orthopedic surgeon WH Kirkaldy-Willis (6), below:
Periarticular Paraphysiological Space Motion
“At the end of the passive range of motion, an elastic barrier of resistance is encountered.”
“If the separation of the articular surfaces is forced beyond this elastic barrier, the joint surfaces suddenly move apart with a cracking noise.”
“This additional separation can only be achieved after cracking the joint and has been labeled the paraphysiological range of motion. This constitutes manipulation.”
“At the end of the paraphysiological range of motion, the limit of anatomical integrity is encountered. Movement beyond this limit results in damage to the capsular ligaments.”
Joint manipulation [adjusting] “requires precise positioning of the joint at the end of the passive range of motion and the proper degree of force to overcome joint [resistance].”
“With experience, the manipulator can be very specific in selecting the spinal level to be manipulated.”
There are a number of benefits from moving joints past the elastic barrier and into the periarticular paraphysiological space range of motion. The best-documented benefit is the reduction of pain. The trick is to move past the elastic barrier and into the periarticular paraphysiological space without exceeding the limit of anatomic integrity. This skill requires training and practice. This is why chiropractors have four years of training, after college, and are licensed by the state.
Ancient History
For millennia humans have known the benefits of optimizing joint motion. The history of joint manipulation parallels the history of civilization. An important review of manipulation through the ages was published in The Journal of Manual & Manipulative Therapy in 2007 and titled (24):
A History of Manipulative Therapy
This review makes these comments:
“Manipulative therapy has known a parallel development throughout many parts of the world. The earliest historical reference to the practice of manipulative therapy in Europe dates back to 400 BCE.”
“Historically, manipulation can trace its origins from parallel developments in many parts of the world where it was used to treat a variety of musculoskeletal conditions, including spinal disorders.”
“It is acknowledged that spinal manipulation is and was widely practiced in many cultures and often in remote world communities such as by the Balinese of Indonesia, the Lomi-Lomi of Hawaii, in areas of Japan, China and India, by the shamans of Central Asia, by sabodors in Mexico, by bone setters of Nepal as well as by bone setters in Russia and Norway.”
“Historical reference to Greece provides the first direct evidence of the practice of spinal manipulation.”
“Hippocrates (460–385 BCE), who is often referred to as the father of medicine, was the first physician to describe spinal manipulative techniques.”
“Claudius Galen (131–202 CE), a noted Roman surgeon, provided evidence of manipulation including the acts of standing or walking on the dysfunctional spinal region.”
“Avicenna (also known as the doctor of doctors) from Baghdad (980–1037 CE) included descriptions of Hippocrates’ techniques in his medical text The Book of Healing.”
“Nobody questions these early origins of manipulative therapy.”
In her 1990 book, Mutant Message Down Under, Marlo Morgan chronicles the journey of a middle-aged, white, American woman with a group of 62 desert Aborigines, across the continent of Australia (25). Morgan chronicled a cultural habit, estimated to be millennia old, at the end of each day’s nomadic journey: members of the group manipulating each other.
Modern History
Prior to the modern era, for hundreds of years in developed and primitive societies throughout the world, practitioners of manipulation were known as bonesetters (24). All of this changed in 1874, and the global seat of change was in the United States of America.
Andrew Taylor Still was a second-generation physician who became disillusioned with medicine following the death (from disease) of three of his children. Dr. Still conceived a theory whereby health could only be maintained and, therefore, disease defeated, by maintaining normal function of the musculoskeletal system (24).
By 1874, “Still referred to himself, in what was a very successful clinical practice, as the ‘Lightening Bone Setter’.” Note this description from reference #24:
“His drugless, non-surgical approach to the treatment of disease rapidly gained acceptance among the general public. He soon found that he was unable to treat the growing numbers of patients and decided he would have to train others to help him in his work.”
“In 1892, he was confident enough in his beliefs that he established the American Osteopathic College in Kirksville, Missouri.”
“He based his theories of disease and dysfunction on the ‘disturbed artery’ in which obstructed blood flow could lead to disease or deformity. This would become known in Osteopathy as the Law of the Artery.”
“As Still’s methods continued to grow in popularity, more colleges were opened and by the time of his death in 1917, 3,000 Doctors of Osteopathy had been graduated.”
The second great addition to the practice of joint manipulation occurred in 1895. Daniel David Palmer was “well educated and an avid reader of all things scientific especially with regard to the healing arts.” Palmer became a self-trained “natural healer.” (24)
With practice experience, “Palmer began to reason that when a vertebra was out of alignment, it caused pressure on nerves.” In 1897, in Davenport, Iowa, Palmer opened his first college, The Palmer College of Cure, now known as the Palmer College of Chiropractic.
In 1907, one the graduates was Palmer’s son Bartlett Joshua or BJ Palmer. In 1910, BJ Palmer introduced the use of X-rays into Chiropractic. Again, reference #24 states:
“The G. I. Bill at the end of World War II enabled thousands of returning soldiers to bolster the ranks of the chiropractic profession.”
“This influx seemed to provide an impetus that would propel the chiropractic profession to today’s status where it boasts 35 schools and colleges worldwide and, in the Western world at least, it is second only to the medical profession as a primary care healthcare provider.”
Summary
Chiropractic-like practitioners have existed throughout history and throughout the world. The evidence suggests that these practitioners exist as a consequence of evolutionary adaptations to protect humans from infections. The fibrotic benefits of walling-off inflammation initiated by infection causes mechanical problems of connective tissues and joints, especially when the inflammation is not infectious, but rather secondary to trauma or stress. Left unmanaged, these joint mechanical deficits impair local biomechanical function, affecting performance, generating pain, and accelerating degenerative changes. Skilled manipulation of these joints improves biomechanical function, reducing pain while improving biomechanical function and performance.
The primary provider of manipulative care today is the chiropractor. Officially started in the year 1895, chiropractic is now recognized and licensed by the federal government, all state governments, and is taught and practiced throughout the world.
REFERENCES:
- Carey N; Epigenetics Revolution: How Modern Biology Is Rewriting Our Understanding of Genetics, Disease, and Inheritance; Columbia University Press; 2013.
- Carey N; Junk DNA: The Journey Through the Dark Matter of the Genome; Columbia University Press; 2017.
- Bredesen DE; Reversal of cognitive decline: A novel therapeutic program; Aging; September 27, 2014; Vol. 6, No. 9; pp. 707-717.
- Bredesen DE, Amos EC, Canick J, Ackerley M, Raji C, Milan Fiala M, Ahdidan J; Reversal of Cognitive Decline in Alzheimer’s Disease; Aging; June 2016; Vol. 8; No. 6; pp. 1250-1258.
- Bredesen DE; The End of Alzheimer’s: The First Program to Prevent and Reverse Cognitive Decline; Avery; 2017.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-540.
- Mehal WZ; Cells on Fire; Scientific American; June 2015; Vol. 312; No. 6; pp. 45-49.
- Boyd W; PATHOLOGY: Structure and Function in Disease; Lea and Febiger; 1952.
- Boyd W; PATHOLOGY: Structure and Function in Disease; Eighth Edition; Lea & Febiger; Philadelphia; 1970.
- Anderson WAD, Scotti TM; Synopsis of Pathology; Ninth Edition; The CV Mosby Company; 1976.
- Robbins SL, Cotran RS; Pathologic Basis of Disease; Second Edition; WB Saunders Company; Philadelphia; 1979.
- Manjo G, Joris I; Cells, Tissues, and Disease; Principles of General Pathology; Second Edition; Oxford University Press; 2004.
- Cyriax, James; Textbook of Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions; Bailliere Tindall; Volume 1; Eighth Edition; 1982.
- Roy, Steven; Irvin, Richard; Sports Medicine: Prevention, Evaluation, Management, and Rehabilitation; Prentice-Hall; 1983.
- Guyton A; Textbook of Medical Physiology; Saunders; 1986.
- Cohen, I. Kelman; Diegelmann, Robert F; Lindbald, William J; Wound Healing, Biochemical & Clinical Aspects; WB Saunders; 1992.
- Korr IM; The Sympathetic Nervous System as Mediator Between the Somatic and Supportive Processes (1970), in The Collected Papers of Irvin M. Korr; American Academy of Osteopathy; 1979; pp. 170-174.
- Cocchiarella L, Anderson GBJ; Guides to the Evaluation of Permanent Impairment; Fifth Edition; American Medical Association; 2001.
- Sandoz R; Some Physical Mechanisms and Effects of Spinal Adjustment; Annals of the Swiss Chiropractic Association; 1976; Vol. 6; pp. 91-141.
- Haldeman S; Modern Developments in the Principles and Practice of Chiropractic; Appleton-Century-Crofts; New York; 1980.
- Kirkaldy-Willis WH; Managing Low Back Pain; Churchill Livingston; (1983 & 1988).
- Kirkaldy-Willis, WH, Cassidy JD; Spinal Manipulation in the Treatment of Low-Back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-40.
- Fischgrund JS; Neck Pain, Monograph 27, American Academy of Orthopaedic Surgeons; 2004.
- Pettman E; A History of Manipulative Therapy; The Journal of Manual & Manipulative Therapy; Vol. 15; No. 3; (2007); pp. 165–174.
- Morgan M; Mutant Message Down Under; 1990.
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

