The escalation in health care spending in the United States has mandated an approach for cost containment. The contemporary approach in this effort is called “Evidenced-Based Medicine.” Proponents of Evidence Based Medicine have become increasingly organized, beginning in the 1990s. As an example, in 1996, the British Medical Journal published an editorial titled (1):
Evidence Based Medicine: What it is and What it isn’t
This article describes Evidence Based Medicine as:
“Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research.”
A necessary component for the implementation of Evidence Based Medicine is the development and use of Clinical Practice Guidelines. As stated in the journal Health Affairs in 2005 (2):
“One common implementation of Evidence Based Medicine involves the use of clinical practice guidelines during medical decision making to encourage effective care.”
A central theme in Evidence Based Guidelines is that treatment should be reasonable and necessary. To establish that treatment is reasonable and necessary, the treating clinician should be using measurement outcomes.
Measurement Outcomes measure the health status of a patient before treatment, and then again after treatment (or a series of treatments) is/are performed. If the post treatment measurement outcome shows improvement, it is classically interpreted that the treatment was both reasonable and necessary. When measurement outcomes stop improving, it means that the patient’s clinical status has reached maximum improvement, or that a different clinical approach may be warranted.
There are literally hundreds of measurement outcomes available for health care providers. Each discipline of health care has developed recognized measurement outcomes that best serve their disciplines and patient’s needs. Chiropractors and other musculoskeletal disciplines often use the same measurement outcomes. These same measurement outcomes that are used clinically are often used in musculoskeletal research. Musculoskeletal health care providers, including chiropractors, commonly use these measurement outcomes:
-
- Oswestry Back Pain Disability Index (ODI)
- Roland-Morris Low Back Pain Disability Questionnaire
- Neck Disability Index (NDI)
- Functional Rating Index (FRI)
- Whiplash Disability Questionnaire
- Headache Disability Index
A sample of each of these is included below.
Clinically, measurement outcomes are primarily used for two purposes:
-
- To show that the treatment given was reasonable and necessary.
- To determine when the patient’s clinical status has reached maximum improvement.
Essentially, if measurement outcomes show progressive improvement in a patient’s clinical status, it means that the treatment given was reasonable and necessary, and that continued treatment is warranted. Additional treatment is warranted as long as the patient’s clinical status continues to improve.
In contrast, if measurement outcomes no longer show improvement, it is often interpreted as meaning that the patient’s clinical status has reached maximum improvement, and additional scheduled treatment may not be warranted. Often, maximum improvement is determined to be when there is no significant change in symptoms and measurement outcomes for approximately 8 weeks (3).
Secondary reasons to use measurement outcomes include:
-
- To document long-term or permanent symptoms and/or disabilities for a particular patient.
- To help apportion treatment, residual symptoms and permanent disabilities.
- The frequency of the use of measurement outcomes is at the discretion of the treating doctor, but here are a few suggestions:
- Appropriate measurement outcomes should be used as a component of initial patient intake.
- For patients under active care, measurement outcomes should be completed at least once per month.
- For patients under maintenance care, measurement outcomes should be completed at least once every 10-12 patient visits.
Measurement outcomes are a standard component of contemporary clinical practice, including for chiropractors. Using measurement outcomes is an invaluable tool for the modern health care provider. Failure to use measurement outcomes invites criticism and conflict. Future health providers will be increasingly judged by their use of measurement outcomes and their results.
••••••••••
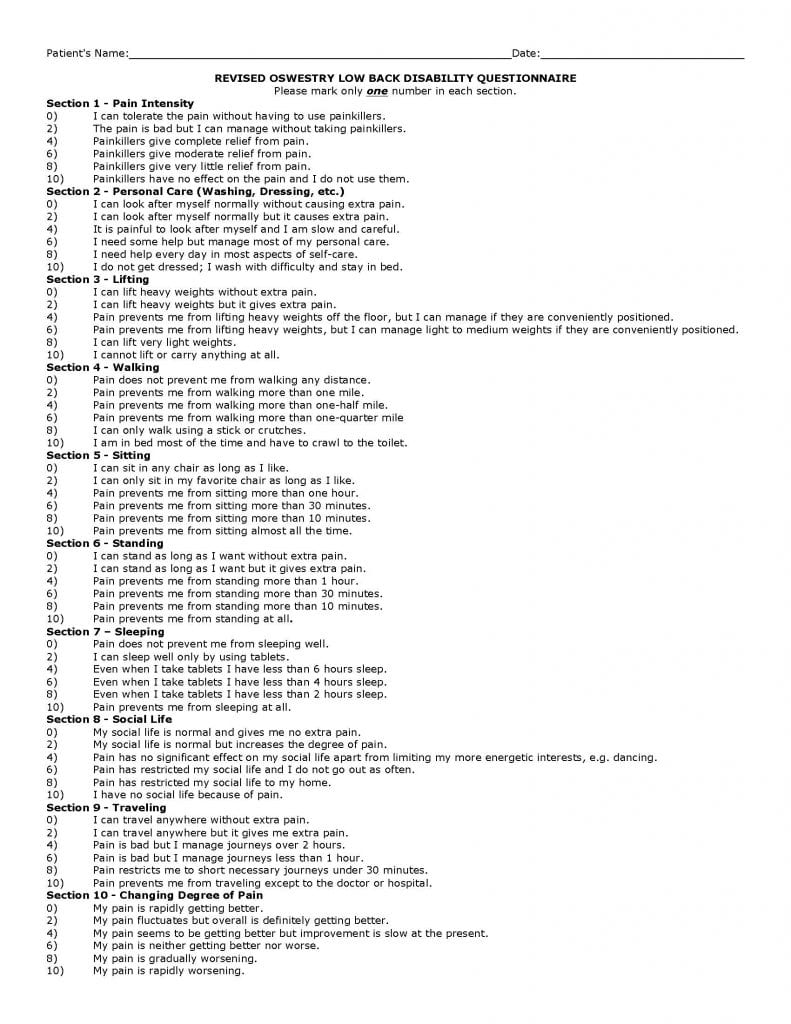
OSWESTRY LOW BACK DISABILITY QUESTIONNAIRE
The Oswestry Low Back Disability was first published in the journal Physiotherapy in 1980 by orthopedic surgeon Jeremy Fairbank, MD, and colleagues from Nuffield Orthopaedic Centre, Oxford, United Kingdom (4).
The Oswestry was revised in 2000 and published in the journal Spine (5).
The Oswestry has become the gold standard for measuring the degree of disability and estimating quality of life in a people with low back pain. The Oswestry is a valid and vigorous outcome measurement (5).
Scoring the Oswestry is as simple as adding the number value on the left side of the form. The total number is the disability index for that patient. The Oswestry disability index is categorized as follows:
0 – 20: Minimal disability
21- 40: Moderate Disability
41 – 60: Severe Disability
61 – 80: Crippling back pain
81 – 100: These patients are either bed-bound or have an exaggeration of their symptoms
••••••••••
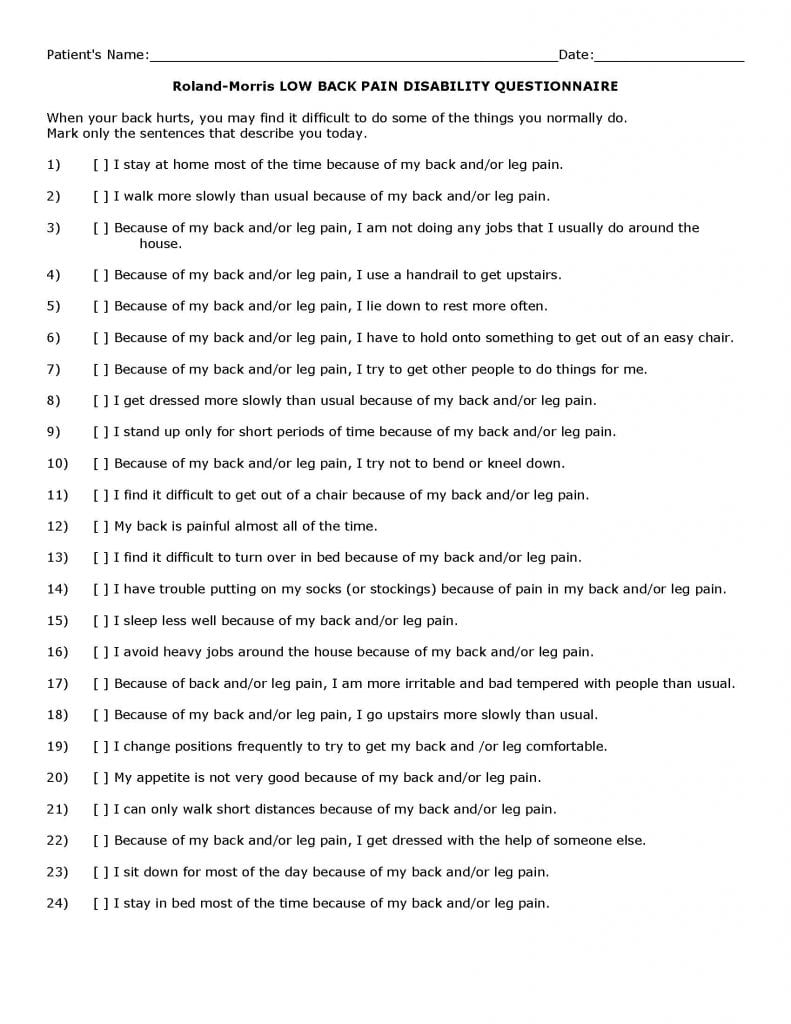
Roland-Morris LOW BACK PAIN DISABILITY QUESTIONNAIRE
The Roland-Morris Questionnaire was first published in the journal Spine in 1983 (6, 7). Professor Martin Roland and colleague R. Morris from the Institute of Public Health at the University of Cambridge developed it. It is longer than the Oswestry, having 24 questions instead of 10. Similarly to the Oswestry, it is considered to be valid and sensitive.
The Roland-Morris Questionnaire is a self-administered. Each of the 24 questions that are checked off is assigned a value of 1. Higher numbers on the 24-point scale reflects greater levels of disability. Clinical improvement over time is graded based on the analysis of serial questionnaire scores. If, for example, at the beginning of treatment, a patient’s score was 18 and, at the conclusion of treatment, his/her score was 8 (10 points of improvement), we would calculate a 55% improvement. [(18-8)/18 x 100]
••••••••••
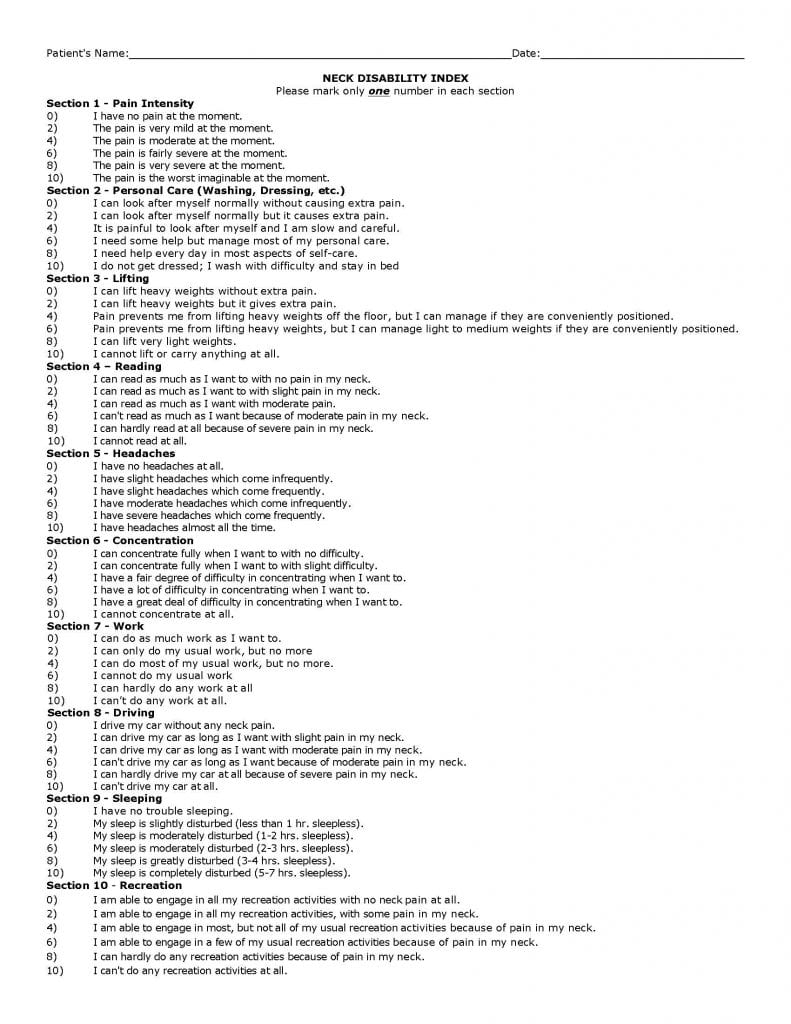
NECK DISABILITY INDEX
The Neck Disability Index was created by chiropractor Howard Vernon, DC, from Canadian Memorial Chiropractic College, Toronto, Ontario, CAN. It was initially published in the Journal of Manipulative ad Physiological Therapeutics in 1991 (8). The initial purpose of the Neck Disability Index was to determine the disability of individuals who had been injured in motor vehicle collisions.
In the construction of the Neck Disability Index, Dr. Vernon modified the Oswestry. It is now the gold standard for measuring the degree of disability and estimating quality of life in a person with neck pain caused my motor vehicle collisions. Similar to the Oswestry, it has been shown to be valid, reliable ad sensitive.
The Neck Disability Index is scored identically to the Oswestry.
••••••••••
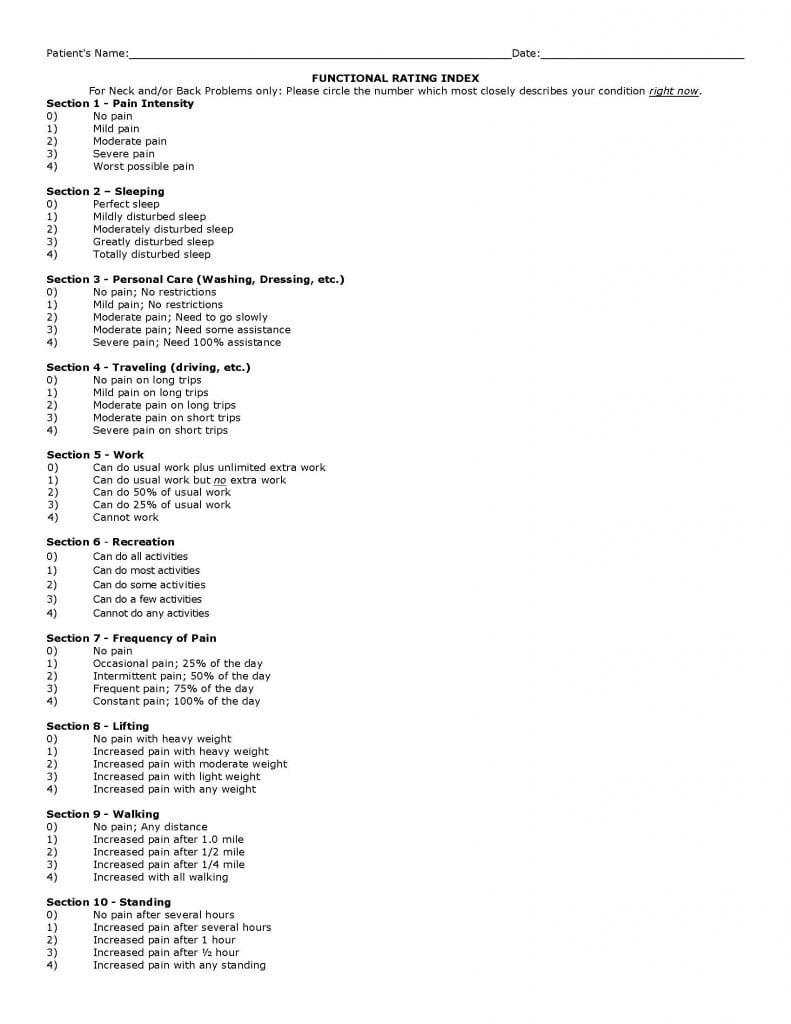
FUNCTIONAL RATING INDEX
The Functional Rating Index is newer, first published in the journal Spine in 2001 (9). The primary authors of the Functional Rating Index are chiropractors Ron Feise, DC, and J. Michael Menke, DC. Dr. Menke is from Palmer Chiropractic College West, located in San Jose, CA.
The Functional Rating Index combines the concepts of the Oswestry Low Back Disability Questionnaire and the Neck Disability Index. It has a total of 10 questions, improving clinical utility (time required for administration).
Their initial study assessed 139 subjects. Their conclusions are:
“The Functional Rating Index appears to be psychometrically sound with regard to reliability, validity, and responsiveness and is clearly superior to other instruments with regard to clinical utility. The Functional Rating Index is a promising useful instrument in the assessment of spinal conditions.”
The Functional Rating Index has 10 questions, and each response is given a value of 0 – 4. Adding up the total score and dividing by 40 determines the percent of disability. If, for example, the summed score is 30, the total disability would be 75%. [30/40 = .75]
If, for example, the Functional Index Score was 10 on a follow-up assessment, the total disability would be 25% [10/40 = .25], and the clinical improvement would be [(30-10)/30 = 67%]
••••••••••
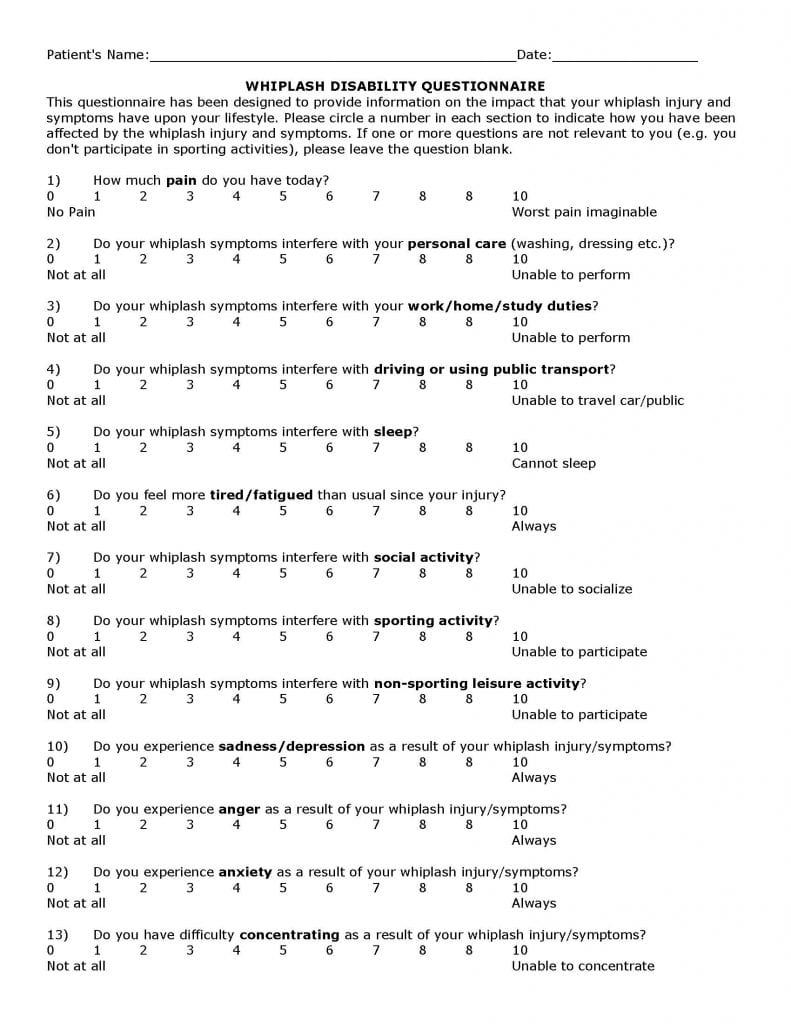
WHIPLASH DISABILITY QUESTIONNAIRE
The Whiplash Disability Questionnaire was first published in the journal Spine in 2004 (10). It was designed by Melanie Pinfold and colleagues from the School of Physiotherapy, La Trobe University, Victoria, Australia. Its reproducibility and responsiveness was further assessed by the same group and published in the journal Pain (11).
-
- The Whiplash Disability Questionnaire measures functional limitations and psychometrics associated with whiplash injury. It was developed from the Neck Disability Index, but it consists of 13 questions rather than 10. The authors concluded:
“The Whiplash Disability Questionnaire has excellent short- and medium-term reproducibility and responsiveness in a population seeking treatment for Whiplash Associated Disorders.”
The Whiplash Disability Questionnaire has 13 questions with a possible of 10 points per question. Scoring is done by adding the total points and dividing by 130.
••••••••••
HEADACHE DISABILITY INDEX
The Headache Disability Index was developed at the Department of Otolaryngology-Head and Neck Surgery, Henry Ford Hospital, Detroit, Michigan. It was first published in the journal Neurology in 1994 (12), and further validated in the journal Headache in 1995 (13).
The Headache Disability Index is 25 questions, and is designed to quantify the impact of headaches on daily living. Each question has only 3 possible responses: YES = 4; SOMETIMES = 2; NO = 0
The authors determined that a 29 point change or greater in the total score from test to retest must occur before the change can be attributed to treatment effects. The authors found the Headache Disability Index to have strong consistency and reliability. They concluded:
“The Headache Disability Index is useful in assessing the impact of headache, and its treatment, on daily living.”

Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

