The human body is designed to effectively absorb and disperse vertical forces. This allows humans to jump off a curb, walk-run-jump, to stuff basketballs and engage in many other sports activities, plop down into a couch, etc., without injury.
In contrast, humans are not well designed to effectively absorb and disperse horizontal forces. The injuries produced by horizontal forces have been recognized for millennia. Horizontal force injuries are predominately attributed to a concept in physics termed inertia.
The laws of physics have always been with us, but they were not formally defined until the year 1687 when Sir Isaac Newton wrote the book Mathematical Principles of Natural Philosophy (1). In this publication, Newton details the principles of inertia.
Inertia is the resistance of a physical object to any change in its state of motion or to its state of rest. An object in motion will remain in motion unless an outside force acts upon that object. Likewise, an object at rest will remain at rest unless an outside force acts upon that object.
Newton’s Laws of Inertia apply to the human body. Different parts of the human body have different inertias between them. It is these inertial differences between the different parts of the body that increase their risk of injury from horizontal forces.
The most important inertia difference in the body is between a human’s trunk and head. The neck (cervical spine) connects these two distinct inertial masses and therefore the neck has a great vulnerability to inertial injury triggered by horizontal forces.
The incidence of neck (cervical spine) inertial injury from horizontal forces dramatically increased with the advent of wheeled transportation. All movements of a wheeled vehicle will move the trunk of the person sitting in the vehicle. Since the trunk inertia is separate from head inertia, the neck is vulnerable to inertial injury.
Wheeled vehicle horizontal force inertial injuries became more evident and understood following the publication of “On Railway and Other Injuries of the Nervous System” more than 150 years ago (2). The primary topic of this publication was horizontal force inertial injuries caused by train collisions and mishaps.
Newton’s concepts of inertia became well known following his publication in 1687. Newton’s Laws would dictate that when a vehicle is struck from behind:
-
- the vehicle is accelerated forward
- the seats in the vehicle are accelerated forward along with the vehicle
- the trunk of the occupant sitting in the seat is accelerated forward along with the seat and the vehicle
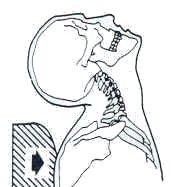
- the head of the occupant, which has different inertia than the trunk, remains at rest while the trunk is accelerated forward; i.e. the trunk is accelerated forward under the stationary head
- the neck, existing between the two larger masses (the trunk and the head), is injured
This would give an appearance of neck extension and/or hyperextension:
Trunk-Head Movement Neck Inertial Injury
It may seem stunning that early publications regarding rear-end motor vehicle collisions appeared to “get it wrong,” backwards. [or did they, discussed below] These early publication stated that during a rear-end motor vehicle collision, the head of the struck vehicle occupant would initially be thrown forward. This would be a violation of Newton’s Laws of Inertia.
As an example, in 1953, physicians James Gay and Kenneth Abbott published an article in the Journal of the American Medical Association, titled (3):
Common Whiplash Injuries of the Neck
These authors studied 50 whiplash-injured patients with symptoms and findings characteristic of a sprain of the neck. They state:
“Collision from behind thrusts body in position of acute flexion, with maximum stress at lower cervical and lumbar spinal regions.”
Drs. Gay and Abbott were quickly rebutted and the mechanisms of rear-end collision inertia were “set straight.” (4) Physician Kirk Cammack, noted in 1957 that early whiplash publications seemed to be unfamiliar with Newton’s laws of motion, believing that the first phase of a rear-end collision was flexion. Dr. Cammack clearly notes that the first phase of a rear-end collision is extension, and he criticizes other earlier studies that appear to have gotten it incorrect.
Soon, the best reference texts pertaining to rear-end motor vehicle collisions also corrected the earlier error: the first phase of a rear-end motor vehicle collisions is extension/hyperextension of the struck vehicle’s occupants head (5, 6, 7).
But What If Everyone Got It Wrong?
Clarifications of rear-end collision biomechanics began in 1991-1995 by Biodynamic Research Corporation, San Antonio, TX. In their 1995 paper, Whitman McConnell and colleagues subjected seven healthy fully informed male human volunteers to rear-end impact velocity changes between 3.6 to 6.8 mph (8). Prior to the testing, each subject’s voluntary cervical spine extension range of motion was measured. During the collision, motion beyond this voluntary range of motion (hyperextension) was never observed in any of the human test exposures. Yet, the authors noted: “All test subjects reported some test related ‘awareness’ or discomfort symptoms,” and most noted fleeting headaches. They concluded that: “Since all of our test subjects, particularly the multiply exposed ones, developed some form of typical ‘whiplash’ symptoms, it seems reasonable to finally conclude that hyperextension was not the cause of their symptoms.”
This challenge to the decades-long belief in the initial inertial extension/hyperextension during a rear-end motor vehicle collision began the new era in whiplash understanding. The basic premise is this:
There is an important biomechanical difference between having one’s shoulders still and moving the head/neck backwards into extension, v. having the head still (Newton’s Laws) and pushing the trunk and neck forward under the stationary head.
To further investigate whiplash rear-end collision biomechanics, in 1997 researchers from Yale School of Medicine began a series of whiplash experiments using fresh human cadaver cervical spines and subjected them to various magnitudes of trauma classes, using an apparatus that simulates rear-end car collisions (9). They captured their findings using high-speed cineradiography which were subsequently digitized. This method of investigation allowed the authors to assess cervical spinal segmental motion rather than the cervical global assessment performed by McConnell and associates in 1995.
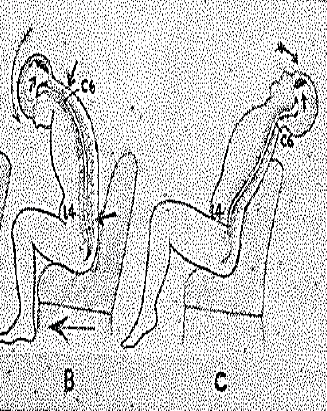
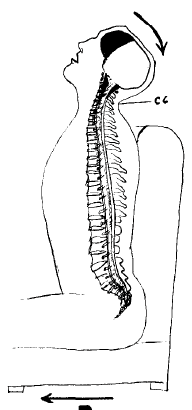
The researchers found that during the rear-end collisions sequence, the head remains stationary as a consequence of its inertia, exactly conforming to Newton’s Laws of Inertia. Since the vehicle occupant’s upper back is in contact with the vehicle’s seat, as the vehicle moves forward during the collision the cervical spine begins extending from the lower cervical spine. But, at the same time, the upper cervical spine and occiput would go into flexion. Hence, with the lower neck in extension and the upper neck in flexion, the cervical spine will initially form an “S” configuration. Continued similar research has confirmed these findings (10, 11, 12).
The greatest criticism of these studies has been the use of cadaver spines rather than living human volunteers. The basic premise is that cadaver spines would not behave the same as a live-human spine; there would be meaningful differences in stiffness, reflexes, etc. That criticism was solved in 1999 (13).
In 1999, researchers from Japan used ten healthy male volunteers who were subjected to a simulated rear-end collision. The motion of the cervical spine was again recorded using cineradiography. The cineradiography images were digitized for the segmental motion analysis.
The authors considered using live human volunteers as the only way to reproduce the passenger’s neck response accurately during a collision, despite the subject’s anticipation of the impact and the restricted impact speed.
The results on these live human volunteers confirmed that initially the upper motion segments went into flexion, and the lower segments into extension; the cervical spine took an S-shaped configuration.
•••••
Protection against the cervical spine “S” configuration during the rear-end motor vehicle collision primarily addresses the position of the head restraint (head-rest). In 2011, the journal Traffic Injury Prevention, published a study titled (14):
Head Restraint Backset During Routine Automobile Driving:
Drivers Usually Exceed the Recommended Guidelines
The authors were from the Joint Biomechanics Laboratory, School of Kinesiology, The University of Western Ontario, Canada. Their purpose was to measure the head restraint distances during routine automobile driving. They note that head restraints were introduced in the late 1960s to limit differential movement of the head and torso, in the hope of reducing spinal motion.
The average head-to-restraint distance throughout the driving route was about 3 inches. In 2007, the National Highway Traffic Safety Administration established that the distance between the back of the head and the head restraint should not exceed 2 inches. Eighty-six percent of the study subjects had average backset distances that exceeded the National Highway Traffic Safety Administration and the Federal Motor Vehicle Safety Standard guidelines, indicating that most drivers may be at risk for whiplash-like disorders if exposed to a rear impact while driving. The authors state:
“If an occupant’s head is unsupported in a rear-end collision, then it lags behind and retracts posteriorly relative to the thorax, resulting in a S-shaped spinal curvature characterized by flexion in upper and extension in lower cervical regions.”
“Properly adjusted head restraints reduce incidence of whiplash injuries.”
“Improper positioning of head restraints appears to be an ongoing issue, because our overall average backset result was significantly higher than the National Highway Traffic Safety standard.”
•••••
In 2014, a thorough review article was published in the journal Turk Neurosurgery, titled (15):
Biomechanics of Neck Injuries
Resulting from Rear-End Vehicle Collisions
The study originated from Koc University, School of Medicine, Departments of Mechanical Engineering and Neurosurgery, Istanbul, Turkey.
The authors note that an important injury prevention factor is the seat’s headrest. Most head restraints are not adjusted to effectively prevent injury.
The distance between the headrest and the head plays a vital role in influencing a whiplash injury. The authors note that head restraints can mitigate whiplash soft tissue injuries, but ideally, they should be less than ¼ inch behind the head, and should not be greater than ½ inch behind the head.
In agreement with other studies, the authors point out that whiplash injuries occur when the cervical spine takes the shape of an “S,” with flexion of the upper cervical spine and extension of the lower cervical spine.
•••••
Most recently (June 2021), a study was published in the Journal of Osteopathic Medicine, titled (16):
Assessment of Potential Strain Injury to Rectus Capitis Posterior Minor Muscles
During Whiplash Type Distortions of the Cervical Spine
The authors of this study are from Michigan State University. Their study specifically evaluated the magnitude of stretch to the rectus capitis posterior minor muscle during the initial flexion of the upper cervical spine during a rear-end motor vehicle collision, and they evaluated how the stretch was affected by the distance between the back of the subject’s head and the vehicle’s head restraint.
Posterior View
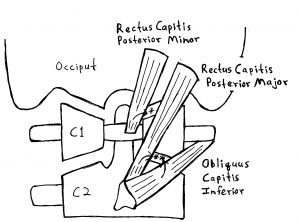
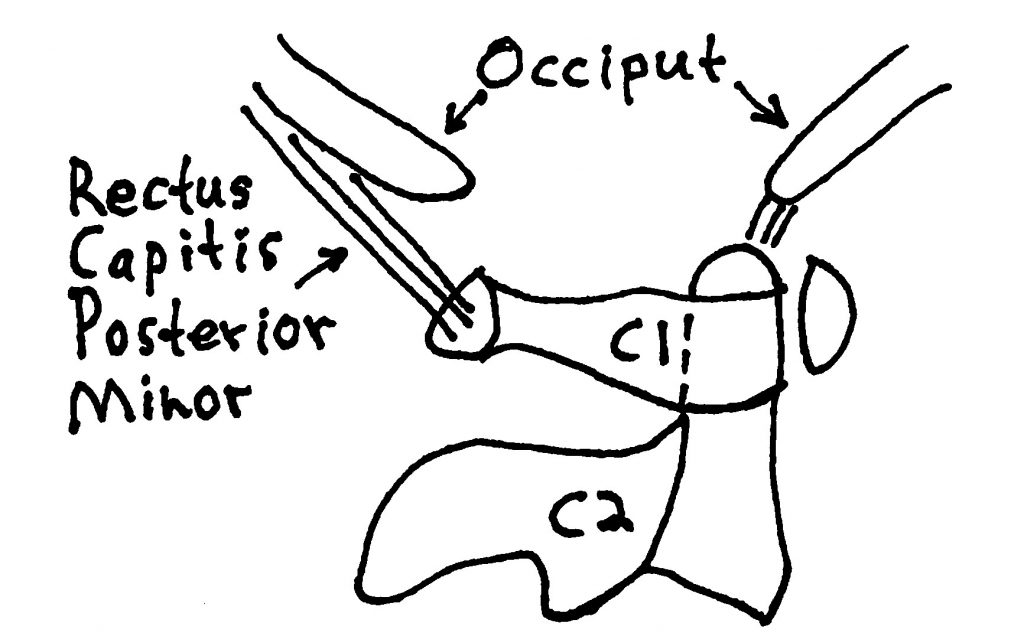
As shown above, the rectus capitis posterior minor muscle originates from the posterior tubercle of the atlas (C1), ascends posterior and superior to attach to the occiput bone behind the foramen magnum. Thus, the muscle crosses the occipitoatlantal joint.
Highly important, the authors emphasize the existence of a strong anatomical connective tissue bridge between the rectus capitis posterior minor muscle and the dura mater of the spinal cord. The existence and importance of the connective tissue bridge between the rectus capitis posterior minor muscle and the dura mater has been emphasized in numerous publications (17, 18, 19, 20, 21, 22, 23).
This anatomical connective tissue bridge has great clinical significance for those injured in a rear-end motor vehicle collision. The authors note:
“On impact, the seat propels the driver’s torso forward relative to the head, resulting in forced flexion of the occipitoatlantal joint, accompanied by forced stretching of the rectus capitis posterior minor muscles.”
“Flexion of the occipitoatlantal joint and stretching of the rectus capitis posterior minor muscles continues to increase until the vehicle’s headrest strikes the back of the driver’s head.”
The backset is the distance between the driver’s head and the head restraint (head rest) at the moment of vehicle collision. The greater the backset, the greater the stretch (strain) on the rectus capitis posterior minor muscles. Backset greater than 2.8 inches resulted in tearing of a few muscle fibers to complete rupture of the muscle and separation of the tendon at the posterior process of C1.
These authors make these points:
Electromyographic evidence shows that the rectus capitis posterior minor muscles “stabilize the occipitoatlantal joint by helping maintain congruency of the joint surfaces.”
Flexion of the occipitoatlantal joint during the initial phase of a rear-end motor vehicle accident “results in a characteristic S-shaped curve resulting from flexion at the occipitoatlantal joint and extension at the lower levels of the cervical spine.”
“Muscle strain injury to the rectus capitis posterior minor muscle is directly related to the magnitude of occipitoatlantal joint flexion.”
“Increasing levels of tissue damage are significant when considering the functional tissue link that interconnects rectus capitis posterior minor muscles to the pain sensitive spinal dura.”
“Muscle strain injury would be expected to impact the functional relationship between the rectus capitis posterior minor muscles and the pain sensitive spinal dura.”
“It is certain that structural damage to the rectus capitis posterior minor muscles would have an adverse effect” on the functional relationship with the myodural bridge.
“A [rectus capitis posterior minor] muscle strain injury would be expected to significantly impact the functional relationship between the rectus capitis posterior minor muscles and the pain sensitive spinal dura.”
“The results of our study revealed that high levels of muscle strain, consistent with whiplash distortions, cause tearing of rectus capitis posterior minor muscle fascicles and separation of the tendon at the posterior process of C1.”
“Cervicogenic pain patients who have experienced whiplash associated with rear-end motor vehicle accident may show clinically relevant structural damage to the rectus capitis posterior minor muscles on MRI.”
These authors note that the risk of a whiplash type injury is directly related to the backset and to the intensity of the impact. The National Highway Traffic Safety Administration guidelines recommend that the backset not exceed 2 inches. Yet, these authors note that a backset of 2 inches produced a 24% strain on the rectus capitis posterior minor muscles, an injurious event. Consequently, the backset should be less than 2 inches. One study (15) advocates that the backset should not exceed ½ inch and that an optimal backset is ¼ inch.
These authors emphasize that a backset recommendation of 2 inches by the National Highway Traffic Safety Administration guidelines would result in a 24% strain on the rectus capitis posterior minor muscles; yet they found that the backset in the typical driver was at 3 inches. A backset of 3 inches exceeds the National Highway Traffic Safety Administration guidelines and would exceed the 30% injury threshold for skeletal muscle strain reported in prior studies. The authors note:
“For values of backset greater than 2.8 inches, whiplash distortions have the potential to result in muscle strain injuries that would range from the tearing of a few muscle fibers to complete rupture of the muscle and separation of the tendon at the posterior process of C1.”
These authors also note that MRI is sufficient to evaluate the fine structures within the occipitoatlantal interspace, diagnosing muscle strain injury to rectus capitis posterior minor muscles. However, they state:
“Unfortunately, the standard clinical protocol for the cervical spine does not include the occipitoatlantal interspace, and the relatively high cost of MRI has restricted its use as a diagnostic tool.”
Consequently, rear-end collision muscle strain injury to rectus capitis posterior minor muscles resulting in dural irritation, inflammation and symptomatology is underdiagnosed.
The authors conclude that the most important thing to protect oneself from rear-end collision injuries to the upper cervical spine is to have one’s head as close as possible to the head restraint (headrest). They state:
“Our model shows that reducing backset, either by adjusting the headrest or reducing forward head posture while driving, should reduce the risk of a strain injury to the rectus capitis posterior minor muscles from a rear-end motor vehicle accident.”
“The results of our study demonstrate that reducing the distance between the driver’s head and the headrest at the time of vehicle impact is an important factor in protecting rectus capitis posterior minor muscles from muscle strain injury.”
“Cervicogenic pain patients who have experienced whiplash-type injuries associated with a rear-end motor vehicle accident may show clinically relevant structural damage to the rectus capitis posterior minor muscles on MRI that may account for the difficulty in managing their pain.”
MANAGEMENT
For the management of rear-end collision muscle strain injury to rectus capitis posterior minor muscles resulting in dural irritation, inflammation and symptomatology, these authors recommend 3 treatments:
-
- Head retraction range-of-motion exercises.
These exercises have a beneficial effect for patients with head and neck pain.
-
- Extension strengthening exercises of the rectus capitis posterior minor muscles.
They state:
“Increased rectus capitis posterior minor muscle strength would be expected to restore normal musculoskeletal functionality of this critical component of the upper cervical spine, with a commensurate decrease in headache pain and forward head posture.”
-
- The use of upper cervical spine manipulation.
This approach to management is consistent with many others who advocate early mobilization, strengthening exercises, and chiropractic manipulation (24, 25, 26, 27, 28, 29).
REFERENCES
- Newton I; Mathematical Principles of Natural Philosophy; July 5, 1687.
- Erichsen JE; On Railway and Other Injuries of the Nervous System; Philadelphia, PA; Henry C. Lea; 1867.
- Gay JR, Abbott KH; Common Whiplash Injuries of the Neck; Journal of the American Medical Association; August 29, 1953; Vol. 152; No. 18; pp. 1698-1704.
- Cammack KV; Whiplash Injuries to the Neck; American Journal of Surgery; April 1957; Vol. 93; pp. 663-666.
- Jackson R; The Cervical Syndrome; Thomas; 1978.
- Foreman S, Croft A; Whiplash Injuries: The Cervical Acceleration / Deceleration Syndrome; Williams & Wilkins; 1988.
- Tollison CD, Satterthwaite JR, editors; Painful Cervical Trauma Diagnosis and Rehabilitative Treatment of Neuromusculoskeletal Injuries; Williams and Wilkins; 1992.
- McConnell WE, Howard RP, Van Poppel J, Karuse R, Guzman HM, Bomar JB, Raddin JH, Benedict JV, Hatsell CP; Human Head and Neck Kinematics After Low Velocity Rear-end Impacts: Understanding “Whiplash”; Society of Automobile Engineers; 1995; pp. 215-238; paper 952724.
- Grauer JN, Panjabi MM, Cholewicki J, Nibu K, Dvorak J; Whiplash Produces a S-shaped Curvature of the Neck with Hyperextension at Lower Levels; Spine; November 1, 1997; Vol. 22; No. 21; pp. 2489-2494.
- Panjabi MM, Cholewicki J, Nibu K, Babat LB, Dvorak J; Simulation of whiplash trauma using whole cervical specimens; Spine; January 1, 1998; Vol. 23; No. 1; pp. 17-24.
- Panjabi MM, Nibu K, Cholewicki J; Whiplash Injuries and the Potential for Mechanical Instability; European Spine Journal; 1998; Vol. 7; pp. 484-492.
- Panjabi MM, Cholewicki J, Nibu K, Grauer J, Vahldiek M; Capsular Ligament Stretches During in Vitro Whiplash Simulations; Journal of Spinal Disorders; June 1998; Vol. 11; No. 3; pp. 227-732.
- Kaneoka K, Ono K, Inami S, Hayashi K; Motion Analysis of Cervical Vertebrae During Whiplash Loading; Spine; April 15, 1999; Vol. 24; No. 8; pp. 763-770.
- Shugg JA, Vernest K, Dickey JP; Head Restraint Backset During Routine Automobile Driving: Drivers Usually Exceed the Recommended Guidelines; Traffic Injury Prevention; April 12, 2011; Vol. 12; No. 2; pp. 180–186.
- Deniz U. Erbulut DU; Biomechanics of Neck Injuries Resulting from Rear-End Vehicle Collisions; Turk Neurosurgery; 2014; Vol. 24; No. 4; pp. 466-470.
- Hallgren RC, Rowan JJ; Assessment of Potential Strain Injury to Rectus Capitis Posterior Minor Muscles During Whiplash Type Distortions of the Cervical Spine; Journal of Osteopathic Medicine; June 4, 2021 [epub].
- Hack G, Koritzer R, Robinson W, Hallgren R, Greenman P; Anatomic Relation Between the Rectus Capitis Posterior Minor and the Dura Matter; Spine; December 1, 1995; Vol. 20; No. 23; pp. 2484-2486.
- Rutten HP, Szpak K, van Mameren H, Ten Holter J, deJong J; Letters: comment on Anatomic Relation Between the Rectus Capitis Posterior Minor and the Dura Matter; Spine; April 15, 1997; Vol. 22; No. 8; pp. 924-926.
- Alix ME, Bates DK; A proposed etiology of cervicogenic headache: the neurophysiologic basis and anatomic relationship between the dura mater and the rectus posterior capitis minor muscle; Journal of Manipulative and Physiological Therapeutics; October 1999; Vol. 22; No. 8; pp. 534-539.
- Hack GD, Hallgren RC; Chronic headache relief after section of suboccipital muscle dural connections: a case report; Headache; January 2004; Vol. 44; No. 1; pp. 84-89.
- Nash L, Nicholson H, Lee ASJ, Johnson GM, Zhang M; Configuration of the Connective Tissue in the Posterior Atlanto-Occipital Interspace; Spine; June 15, 2005; Vol. 30; No. 12; pp. 1359-1366.
- Scal F, Marsili ES, Pontell ME; Anatomical Connection Between the Rectus Capitis Posterior Major and the Dura Mater; Spine; December 1, 2011; Vol. 36; No. 25; pp. E1612–E1614.
- Zheng N, Yuan XY, Li YF, Chi YY, Gao HB, Zhao X, et. al.; Definition of the To Be Named Ligament and Vertebrodural Ligament and Their Possible Effects on the Circulation of CSF; Public Library of Science ONE; August 1, 2014; Vol. 9; No. 8; pp. e103451.
- Kellett J; Acute Soft Tissue Injuries–A review of the Literature; Medicine and Science in Sports and Exercise; October 1986; Vol. 18; No. 5; pp. 489-500.
- Kannus P; Immobilization or Early Mobilization After an Acute Soft-Tissue Injury?; The Physician And Sports Medicine; March 2000; Vol. 26; No. 3; pp. 55-63.
- Rosenfeld M, Gunnarsson R, Borenstein P; Early Intervention in Whiplash-Associated Disorders: A Comparison of Two Treatment Protocols; Spine; July 15, 2000; Vol. 25; pp. 1782-1787.
- Hoving JL, Koes BW, de Vet HCW, van der Windt DAWM, Assendelft WJJ, van Mameren H, Devillé WLJM, Pool JJM, Scholten RJPM, Bouter LM; Manual Therapy, Physical Therapy, or Continued Care by a General Practitioner for Patients with Neck Pain: A Randomized, Controlled Trial; Annals of Internal Medicine; May 21, 2002; Vol. 136; No. 10; pp. 713-722.
- Woodward MN, Cook JCH, Gargan MF, Bannister GC; Chiropractic Treatment of Chronic ‘Whiplash’ Injuries; November 1996; Injury; Vol. 27; No. 9; pp. 643-645.
- Khan S, Cook J, Gargan M, Bannister G; A symptomatic classification of Whiplash Injury and the Implications for Treatment; The Journal of Orthopaedic Medicine; 1999; Vol. 21; No. 1; pp. 22-25.
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

