A Common Sequela Of Neck Injuries
In 1991, Denver Thoracic Outlet surgeon Richard Sanders, MD, wrote a book with the above title (1). In this months issue we are going to discuss many of Dr. Sanders’ remarkable observations… beginning with…
His Definition of Thoracic Outlet Syndrome (TOS)
“TOS is neurovascular symptoms in the upper extremity due to pressure on the nerves and vessels in the thoracic outlet area. The specific structures compressed are usually the nerves of the brachial plexus and occasionally the subclavian artery or subclavian vein.”
Synonyms for TOS include brachiocephalic syndrome, cervicobrachial syndrome, and cervicothoracic syndrome.
Mechanisms
Scalene muscle injury, secondary to cervical spine trauma, is the commonest etiology of thoracic outlet syndrome. In some studies, trauma was the cause of TOS in 86% of patients, and automobile accidents were the commonest type of injury. Anatomically, the scalene muscles normally touch the nerves of the brachial plexus.
A typical breakdown of etiology, from Dr. Sanders (1), is as follows:
| Trauma | 86% | ||
| Rear-end MVC | 32% | ||
| Front or Side MVC | 24% | ||
| Work Injury | 20% | ||
| Work Stress Injury | 2% | ||
| Other Trauma | 8% | ||
| Cervical Rib | 2% | ||
| Axillary Vein Occlusion | 1% | ||
| Arterial Insufficiency | 1% | ||
| Soft Tissue Other Than Trauma | 10% |
In studies in which every patient is asked if an accident or injury to the neck preceded the onset of TOS symptoms, the incidence of trauma increased to 91%.
The cervical spine trauma that causes TOS “need not be of great severity.”
Dr. Sanders (1) further notes:
“In the large majority of patients, the onset of TOS symptoms follows neck injury and is accompanied by head and neck complaints as well as extremity symptoms. It is easy to explain the symptoms of TOS as the result of scalene muscle injury followed be scarring, tightening or spasm of the scalenes, and subsequent compression of the plexus.”
“Over 80% of patients with TOS have a history of some type of trauma preceding the onset of their illness.” “The usual cause is an auto accident, most often a rear-end collision, but impacts from the front or side are fairly frequent causes. The common denominator is acute hyperextension of the neck (whiplash injury).”
In 2001, Ide and colleagues (2) from the Department of Orthopaedic Surgery, Kumamoto University School of Medicine, Japan, investigated the incidence of brachial plexus irritation in 119 patients with whiplash injuries. They concluded that the primary injury to the thoracic outlet/brachial plexus nerves was a stretching injury. They noted that these thoracic outlet/brachial plexus injuries occur in a significant proportion of patients after a whiplash injury, and are associated with a poor outcome.
Cervical ribs are a predisposing factor rather than the primary cause of thoracic outlet syndrome. No more than 10% of people with cervical ribs ever develop thoracic outlet syndrome symptoms. Those who do become symptomatic usually relate the onset of symptoms to some type of trauma.
Congenital bands and ligaments are also found attached to the first rib in some patients with thoracic outlet syndrome. While the ligaments have been present since birth, it usually requires neck injury to elicit symptoms. It is the injury, rather than the congenital band, that is the immediate cause of the thoracic outlet syndrome.
Risk factors for the development of post-traumatic thoracic syndrome include a longer neck, cervical kyphotic malalignment, and sloping shoulders (3). An assessment of the biomechanics of cervical risk factors can be done radiographically. Increased risk factors for post-traumatic thoracic outlet syndrome included long cervical spine, narrowed central neural canal, and reduced cervical lordosis. The measurements were made as follows (3):
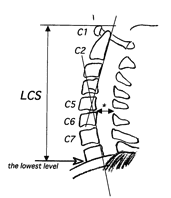
The radiographic measurements of neutral lateral view included:
(1) The lowest level of vertebral body.
(2) LCS (length of cervical spine) measured from the tip of the superior margin at C1 to the lowest level.
(3) Anterior–posterior canal diameter of C5–C6 (*).
(4) Cervical lordotic angle formed by straight line at posterior margin of C2 and C7.
Types Of Thoracic Outlet Syndrome
There are two primary types of thoracic outlet syndrome, Neurogenic and Vascular. Neurogenic thoracic outlet syndrome compromises more than 95% of cases. Vascular thoracic outlet syndrome compromises less than 5% of cases.
The vascular symptoms of thoracic outlet syndrome are more often arterial than venous. Arterial thoracic outlet syndrome is compression of the subclavian artery in the region of the scalene triangle and costoclavicular space. The artery can also be afflicted by aneurysm, thrombosis, or emboli. Arterial thoracic outlet syndrome is uncommon, occurring in less than 5% of all cases of thoracic outlet syndrome, and usually in less than 1-2% of cases. Although small in absolute numbers, arterial thoracic outlet syndrome accounts for a large percentage of the serious disabilities resulting from thoracic outlet syndrome. Most cases of arterial thoracic outlet syndrome are associated with a bony abnormality, usually a complete cervical rib. Also, incomplete cervical ribs are usually attached to the first rib by a dense fibrous band that can exert pressure against an arterial wall similar to that imposed by a cervical rib.
The incidence of venous obstruction in all thoracic outlet syndrome patients is small, from 1.5 to 5%. Venous thoracic outlet syndrome symptoms include swelling, cyanosis, and aching.
VASCULAR v. NEUROLOGIC SYMPTOMS
Arterial symptoms include coldness, pallor, Raynauld’s phenomenon (color changes), claudication, and gangrene of fingertips (from emboli). The etiology of such vascular symptoms is usually irritation of the sympathetic nerves accompanying the somatic nerve plexus; therefore they are indicative of neurologic compression. Dr. Sanders (1) states:
“Irritation of the sympathetic nerve fibers that accompany C8 and T1 produce peripheral vasoconstriction and symptoms of coldness, color changes, excessive sweating, and on occasion, even ischemic lesions in the finger tips.”
These symptoms mimic those of arterial emboli, but are usually due not to emboli, but to irritation of the sympathetic nerves. Therefore they are neurologic rather than vascular symptoms.
In 2007, Drs. Richard J. Sanders, Sharon L. Hammond and Neal M. Rao from the Department Surgery, Rose Medical Center, Denver, CO, and the University of Colorado Health Science Center, presented a paper based upon their more than 2,500 thoracic outlet surgeries over a period of 40 years (6). They state:
Arterial TOS Less than 1% of cases
Venous TOS About 3% of cases
Neurogenic TOS Over 95% of cases
Dr. Sanders and colleagues (6, 2007) make the following points:
“Most patients with neurogenic TOS have a history of neck trauma preceding their symptoms, auto accidents being the most common and repetitive stress at work being next most common.”
Venous TOS may be preceded by excessive activity with the arms.
“Symptoms of arterial TOS usually develop spontaneously, unrelated to trauma or work. Arterial TOS is almost always associated with a cervical rib or an anomalous first rib and, thus, a normal neck x-ray is a good screening test to rule out ATOS.”
Cervical ribs occur in less than 1% of the population and most cervical ribs are asymptomatic. “However, the cervical rib is a predisposition to develop Neurogenic TOS following neck trauma, most often whiplash injuries.”
“The only patients we have seen develop arterial TOS had either a complete cervical rib or an anomalous first rib. Since arterial TOS is usually asymptomatic until arterial emboli occur, asymptomatic patients found to have one of these rib anomalies are followed with duplex scans every few years to detect silent arterial abnormalities. If arterial abnormalities develop, surgical repair of the artery and excision of the rib should be performed before arterial TOS develops.”
Symptoms
Typical symptoms of thoracic outlet syndrome are:
Paresthesia in the fingers, hand, or arm. This paresthesia is most common in all five fingers, but it is often worse in the fourth and fifth fingers.
Pain in the upper extremity, shoulder, neck, and sometimes above or along the medial edge of the scapula.
Arm weakness.
Occipital headaches.
Aggravation of the symptoms with the arm elevated.
Chest pain, facial pain, hand swelling, and color changes are seen in a few patients, but are less frequent.
Other documented symptoms from thoracic outlet syndrome include pain in the neck, face, mandible, ear, occipital headaches, dizziness, vertigo, and blurred vision.
While the textbook description of thoracic outlet syndrome describes numbness and tingling in the fourth and fifth digits, more patients have involvement of all five fingers, with the fourth and fifth fingers often being worse.
Dr. Sanders (1) notes:
“Within 24 hours of the injury, headaches, neck pain, and neck stiffness develop. Dorsal spine pain and aching in the shoulders are other early symptoms. Numbness and tingling in the arms and fingers usually do not occur immediately but appear several days, weeks, or sometimes even a few months after the accident. Elevating the arms typically elicits or aggravates the symptoms.”
RECENT SYMPTOM NUMBERS, 223 CASES (1)
History of Trauma 91%
Arm Paresthesias 90%
Neck Pain 85%
Headache 83%
Arm Pain 74%
Shoulder Pain 68%
Arm Weakness 29%
Chest Pain 9%
Facial Pain 4%
Raynaud’s Phenomenon 2%
Arm Swelling 1%
Dr. Sanders and colleagues in 2007 (6) make the following symptomatic divisions:
Arterial TOS Symptoms
The symptoms of ATOS include digital ischemia, claudication, pallor, coldness, paresthesia, and pain in the hand but seldom in the shoulder or neck. These symptoms are the result of arterial emboli or from thrombus forming just distal to subclavian artery stenosis. The pallor and coldness are due to arterial ischemia.
Venous TOS Symptoms
“Swelling of the arm, plus cyanosis, is strong evidence of subclavian vein obstruction, either thrombotic or nonthrombotic. Pain or aching is often present, but may also be absent. The arm swelling seen in VTOS is not a feature of either ATOS or NTOS. Paresthesia in the fingers and hands is common in venous TOS and may be secondary to swelling in the hand rather than to nerve compression in the thoracic outlet area.”
Neurogenic TOS Symptoms
“Pain, paresthesia, and weakness in the hand, arm, and shoulder, plus neck pain and occipital headaches, are the classical symptoms of NTOS. Raynaud’s phenomenon, hand coldness and color changes, is also frequently seen.”
Pathology
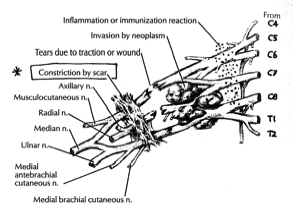
Any entity that causes swelling and/or fibrosis of the scalene muscles can elicit symptoms of thoracic outlet syndrome. Since 1990, histochemical studies have demonstrated fiber changes as well as scar tissue in both anterior and middle scalene muscles of thoracic outlet syndrome patients. Histological studies show increased connective tissue in the scalenes of most thoracic outlet syndrome patients. Trauma caused inflammation, fibrosis and contracture of the anterior scalene muscle, compresses the brachial plexus and subclavian artery to produce thoracic outlet syndrome symptoms.
Dr. Sanders (1) notes:
“Injury to the scalenes results in muscle fibrosis and mild plexus compression by tightened or spastic anterior and middle scalene muscles. The scalene muscles might compress the nerves of the brachial plexus when they contract, given that fibrosed muscle would be less flexible than normal.”
In 2005, Schenardi (4) notes:
“Injury can cause a fibrosis of the plexus because of the change of microenvironment of the nerves.”
Post-traumatic edema stimulates the “production of connective tissue which eventually might lead to endoneurial scar tissue.”
When the neck in hyper-extended, “the scalene muscles, which hold the neck in place, are torn, causing blood and other fluids to leak into the brachial plexus injury. This causes scar tissue in the brachial plexus.”
Also in 2005, Alexandre (5) and colleagues confirm that the pathology of thoracic outlet syndrome is “posttraumatic brachial plexus entrapment in fibrotic scarring.” Their operative finding on patients with thoracic outlet syndrome was “moderate to dense scar tissue surrounding completely the offended nerve trunks at the point of their exit from the interscalenic space.” Post-traumatic thoracic outlet fibrotic scar tissue is probably the physical basis for prolonged complaints of patients who suffered from low-speed rear-end accidents. Importantly, the greatest degree of brachial plexus scarring was adhered nerves to the anterior scalene muscle. Therefore, the anterior scalene muscle is an important treatment target.
Post Traumatic Muscle Injury and Fibrosis; Treatment with Transverse Friction, based on Cyriax (7):
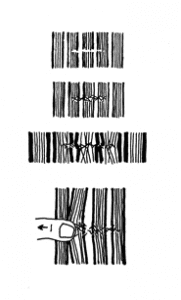
Brachial Plexus Fibrosis From Jones (8):
In 2007, Dr. Sanders and colleagues note (6):
In Neurogenic TOS, the coldness and color changes are due to an “overactive sympathetic nervous system whose fibers run on the circumference of the nerve roots of C8, T1, and the lower trunk of the brachial plexus.”
“When the nerves are irritated or compressed, the sympathetic fibers are activated, producing Raynaud’s phenomenon. This explains how the coldness and color changes are frequently seen with NTOS.”
Diagnosis
Schenardi (4) notes that x-rays, MRI, and CT usually fail to show the pathology in thoracic outlet syndrome, and that electrodiagnostic studies may be normal.
Tight scalene muscles explain the non-neurologic symptoms seen in thoracic outlet syndrome patients, such as neck pain, neck stiffness, and occipital headaches.
Although osseous anomalies are rarely the cause of thoracic outlet syndrome symptoms, their presence can be very important. Therefore, Dr. Saunders recommends that “Cervical Spine x-rays should be obtained in all patients.”
Adson’s test for thoracic outlet syndrome diagnosis has been around since 1927. The patient takes a long deep breath, elevates the chin, and turns the chin to the affected side. A decrease or obliteration of the radial pulse is a sign of scalenes anticus syndrome. However, positive tests occur in over 50% of normal people. Therefore Adson’s test cannot be relied upon in diagnosing thoracic outlet syndrome.
Pulling the shoulders backward and downward to diagnose thoracic outlet syndrome [Eden’s test] has been around since 1943, and is usually positive in costoclavicular syndrome. However, positive tests occur in as high as 68% of normal people. Therefore, this test also cannot be relied upon to diagnose thoracic outlet syndrome.
Dr. Sanders (1) notes that the history is more important than the physical examination in making a diagnosis of thoracic outlet syndrome.
The only two physical findings that are present in over 90% of thoracic outlet syndrome patients are tenderness over the scalene muscles and reproduction of symptoms with the arms abducted to 90 degrees in external rotation (90-degree AER position). Dr. Sanders (1) states:
“The most important aspects of physical examination in establishing a diagnosis of thoracic outlet syndrome are palpation for supraclavicular tenderness [directly over the anterior scalene muscle, 3 cm lateral to the trachea and 2-3 cm above the clavicle] and checking for symptoms with the arms in the 90-degree AER position.”
“The second point to palpate is in the supraclavicular space directly over the brachial plexus, located 1 cm posterior to the anterior scalene muscle. The thumb presses over the plexus, holding pressure for 20-30 seconds. A positive response is the onset of paresthesia or pain radiating to the arm and hand, similar to the patient’s symptoms.”
The 90-degree AER position will reproduce thoracic outlet syndrome symptoms in over 90% of thoracic outlet syndrome patients. Positive responses in normal people occur only 5 – 10% of the time. The neck should be extended while performing this maneuver. The pioneering Thoracic Outlet Surgeon Dr. David Roos describes exercising the fingers in this position. However, studies and experience suggests that a positive response will occur as easily without exercise.
About half of thoracic outlet syndrome patients have weakness of the affected hand. Yet, the majority of thoracic outlet syndrome patients do not have muscle atrophy. Their symptoms are sensory, not motor, and EMG results are usually normal.
Nerve Conduction Velocity testing measures both sensory and motor nerves. Importantly, normal nerve conduction studies do not rule out the diagnosis of thoracic outlet syndrome.
Arterial thoracic outlet syndrome often has a cervical rib on x-ray, or a pulsatile supraclavicular mass with a subclavian bruit with the arm at rest. Unfortunately, the presence of subclavian bruit with positional change is found in many normal people, a fact that renders this sign unreliable for diagnosing thoracic outlet syndrome in the absence of symptoms. However, a history of sudden onset of unilateral extremity symptoms in the absence of trauma should raise suspicion of arterial emboli.
Treatment
Fewer than 25% of the patients seen for thoracic outlet syndrome are operated upon, as most patients are managed conservatively. Conservative management includes control of post-traumatic inflammation, early persistent motion to minimize the adverseness of scar formation and adhesions, and shoulder/neck strengthening and stretching exercises.
There is evidence for a Double Crush component to thoracic outlet syndrome (2, 3, 4). Consequently, appropriate management of cervical spine mechanical problems is essential in the overall management of thoracic outlet syndrome. Studies (3) indicate that the primary Double Crush component of thoracic outlet syndrome is discogenic. Conservative treatment duration for patients with traumatic neurogenic thoracic outlet syndrome can exceed 4 months, and even exceed 1 year if the cervical discs are involved.
Surgery for thoracic outlet syndrome should not be performed until the patient has failed to improve while on conservative management for at least a few months. Dr. Sanders (1) states:
“Surgery is a last resort; conservative treatment should be tried first.”
“If symptoms do not improve with several months of conservative management, the patient regards the symptoms as disabling, and all other treatable conditions have been excluded, the patient must either live with the symptoms or undergo surgery. With surgery not an ideal solution, if there is persistent nerve compression, surgery is the only alternative.”
“Recurrent symptoms develop in 15-20% of patients who have received operations for thoracic outlet syndrome.”
“The almost constant finding at reoperations for thoracic outlet syndrome is the presence of scar tissue around the nerves of the plexus.”
“Scar tissue lies not only around the entire neurovascular bundle, but also around the individual nerves comprising the plexus. Presumably it is the maturation and contraction of this scar tissue that produces brachial plexus compression.”
In 2001, Yukihiro Kai and colleagues (3) indicated that post-traumatic cervical
spine kyphosis is a perpetuating factor in thoracic outlet symptoms. They note that cervical kyphosis will lead to total spinal malalignment, increasing whole body stress and symptoms. They indicate that medical care will not improve the spinal alignment and therefore will not be effective for long-term relief. Consequently, management of cervical kyphosis and related whole body misalignment is important in the treatment of thoracic outlet syndrome.
The late James Cyriax, MD, from the Department of Orthopedic Medicine, St. Thomas’s Hospital in London, and Professor of Orthopaedic Medicine, University of Rochester Medical School, notes in his 1983 text Illustrated Manual of Orthopaedic Medicine, the value of transverse friction in the treatment of post-traumatic muscle fibrosis (7).
Thoracic Outlet Syndrome Questionnaire,
To Be Completed By The Patient
INSTRUCTIONS: Circle YES or NO for each question
Circle RIGHT or LEFT or both RIGHT and LEFT if on both sides
| •Do you have pain in any of these areas? | |||
| Head (Headache) | YES | NO | If yes, BACK or FRONT of head? |
| Neck | YES | NO | RIGHT LEFT |
| Between Shoulders | YES | NO | |
| Shoulders | YES | NO | RIGHT LEFT |
| Elbow | YES | NO | RIGHT LEFT |
| Forearm (below elbow) | YES | NO | RIGHT LEFT |
| Hand | YES | NO | RIGHT LEFT |
| •Do you have numbness or tingling in your? | |||
| Fingers | YES | NO | |
| If YES, circle which fingers: | |||
| RIGHT Hand: | Thumb Index Middle Ring Baby | ||
| LEFT Hand: | Thumb Index Middle Ring Baby | ||
| Forearm (below elbow) | YES | NO | RIGHT LEFT |
| Arm (above elbow) | YES | NO | RIGHT LEFT |
| •Do you have weakness in your hand or arm? | |||
| YES | NO | RIGHT LEFT | |
| •Does elevating your hand over you head make your symptoms worse? | |||
| YES | NO | RIGHT LEFT | |
| •Were you in an accident? | |||
| YES | NO | DATE: | |
| •Where any of your arm symptoms present prior to your accident? | |||
| YES | NO | DATE: | |
| •Where any of your arm symptoms present prior to your accident? | |||
| YES | NO | ||
| •Have you had any other accidents involving your head or neck prior or after this one? | |||
| YES | NO | DATE: | |
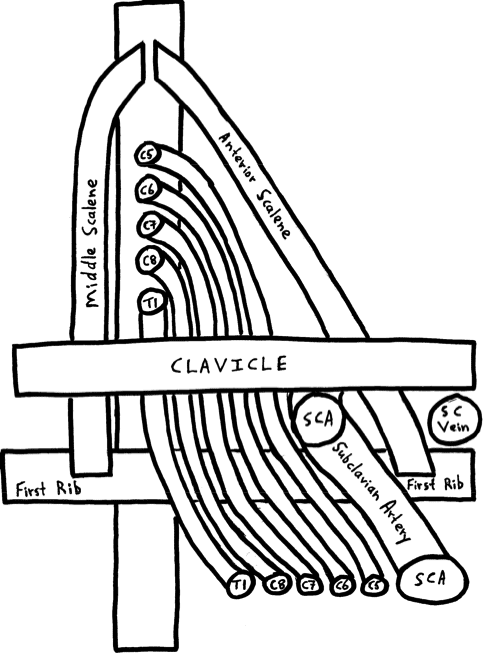
Thoracic Outlet Syndrome
The Scalene Triangle
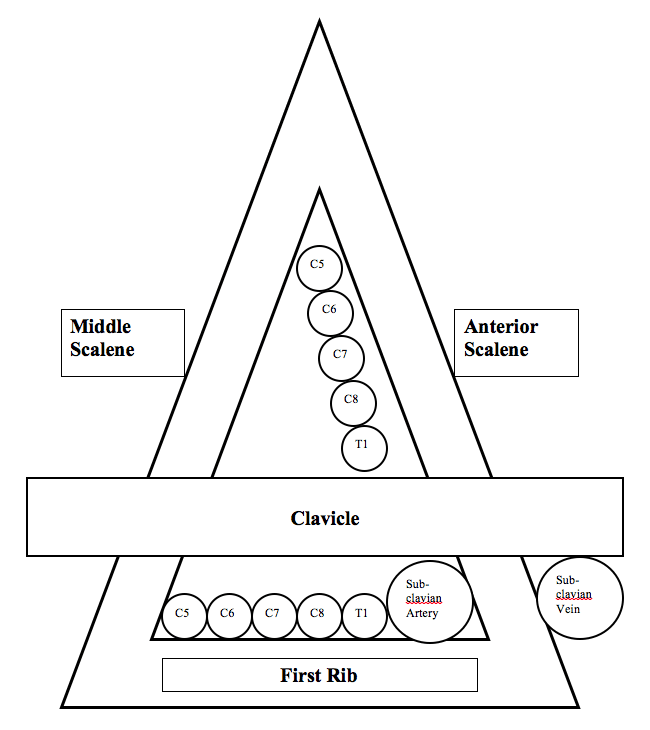
Thoracic Outlet Syndrome; The Scalene Triangle
References
1) Sanders, Richard; Thoracic Outlet Syndrome: A Common Sequela Of Neck Injuries, Sanders, 1991.
2) Ide M, Ide J, Yamaga M, Takagi K; Symptoms and Signs of Irritation of the Brachial Plexus in Whiplash Injuries; Journal of Bone and Joint Surgery (Br); 2001 Mar;83(2):226-9.
3) Yukihiro Kai; Masanobu Oyama; Shinnosuke Kurose; Tatsuro Inadome; Yutaka Oketani; Yoshitake Masuda. Neurogenic Thoracic Outlet Syndrome in Whiplash Injury; Journal of Spinal Disorders, 2001 December;14(6)487-493.
4) Schenardi C; Whiplash injury, TOS and double crush syndrome: Forensic medical aspects; Acta Neurochirurgica, supplement, Vol. 92, 2005, pp. 25-27.
5) Alexandre A, Coro L, Azuelos A, Pellone M. Thoracic outlet syndrome due to hyperextension-hyperflexion cervical injury; Acta Neurochir Supplement, November 29, 2005;92:21-4.
6) Richard J. Sanders MD, Sharon L. Hammond MD and Neal M. Rao BA; Diagnosis of thoracic outlet syndrome; Journal of Vascular Surgery; Volume 46, Issue 3, September 2007, Pages 601-604.
7) Cyriax J and Cyriax P, Illustrated Manual of Orthopaedic Medicine, Butterworths, 1983.
8) Jones HR, Netter’s Neurology, Icon Learning, 2005.
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

