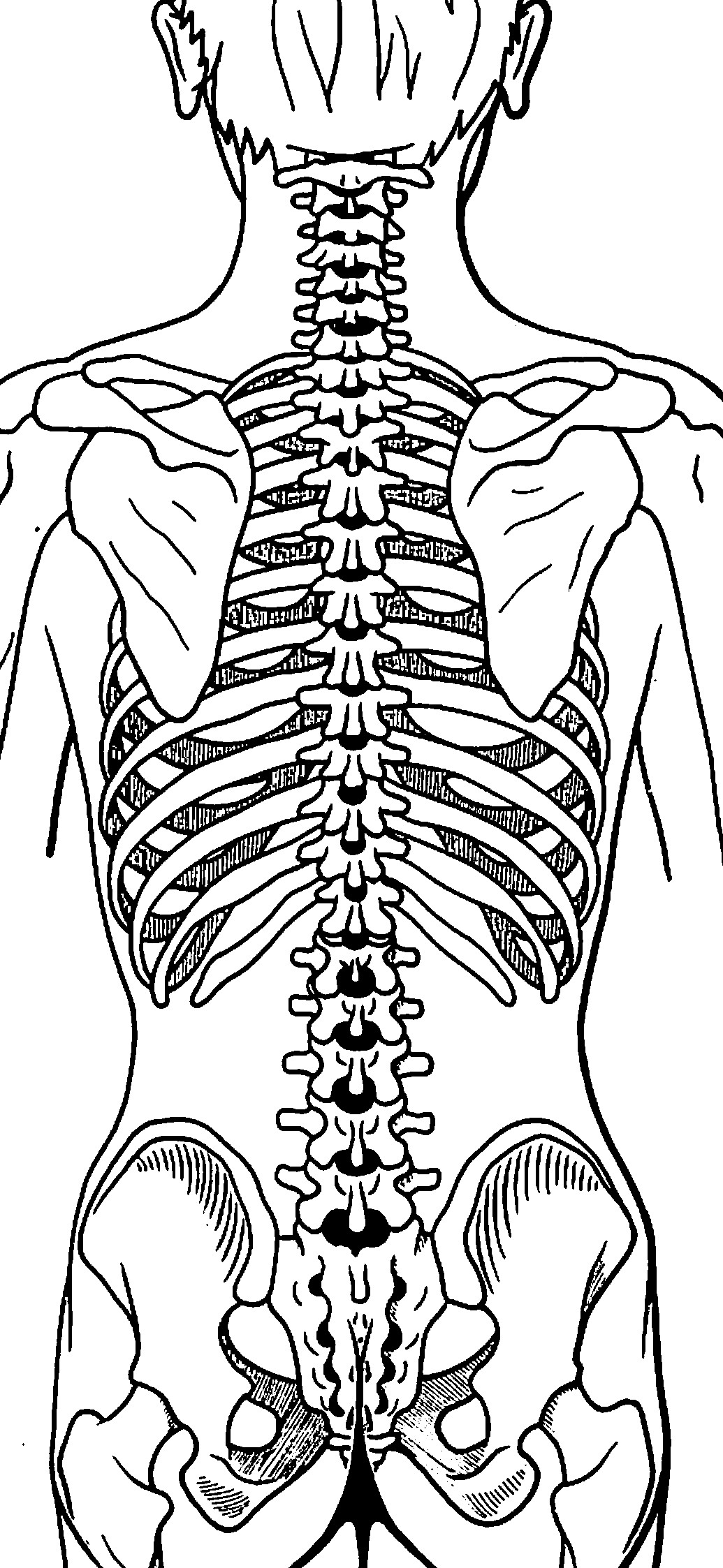
When viewing the human spinal column from directly in front or directly behind, it should be straight and without lateral (sideways) deviation. The health and function of the human spinal column is optimum when there is no lateral (sideways) deviation into the coronal plane. This concept is well-noted by Joel Goldthwait, MD, and well-reviewed by James Oschman, PhD (1):
Gravity is the most potent physical influence in any human life.
“Gravity pervades our bodies and our environment and affects our every activity. All of the structures around us – our homes, furniture, buildings, machinery, plant, and animal, – and our own bodies, are designed to function in a world dominated by gravity.”
“To introduce the therapeutic significance of gravity, we summarize the work of Joel E. Goldthwait and his colleagues at Harvard Medical School.” “A surgeon in Boston and founder of the orthopaedic clinic at the General Hospital, Goldthwait developed a successful therapeutic approach to chronic disorders. The aim of his therapies was to get his patients to sit, stand, and move with their bodies in a more appropriate relationship with the vertical. After years of treating patients with chronic problems, he concluded that many of these problems arise because parts of the body become misaligned with respect to the vertical, and organ functions therefore become compromised.”
“Goldthwait’s therapeutic approach was based in part on observations made while performing surgery on such patients. He noticed that abdominal nerves and blood vessels are under tension in individuals whose bodies are out of alignment. He also reported ‘stretching and kinking’ of the cerebral arteries and veins in those whose necks were bent. Various cardiac problems were correlated with ‘faulty body mechanics’ that distorted the chest cavity in a way that impaired circulatory efficiency. Goldthwait also documented with X-rays a build-up of calcium deposits around the vertebrae of individuals with chronic arthritis, and observed that these deposits can diminish when the individual acquires a more vertical stance. His therapeutic approach corrected many difficult problems without the use of drugs. He viewed the human body from a mechanical engineering perspective, in which alignment of parts is essential to reduce wear and stress. He pleaded with physicians to recognize and correct misalignments to prevent long-term harmful effects.”
“The basic principle of gravitational biology is known to any child who plays with blocks. The center of gravity of each block must be vertically above the center of gravity of the one below, to have a stable, balanced arrangement. If the center of gravity of one block lies outside of the gravity line, stability is compromised.”
“Likewise, there is only one stable, strain-free arrangement of the parts of the human body. Any variation from this orientation will require corresponding compensations in other parts of the support system.”
“Misalignment of any part will affect the whole system, and that restoration of verticality is a way to address a wide variety of clinical problems.”
Dr. Goldthwait pleaded for everyone to pay more attention to the ways they hold and move their bodies in relation to the gravity field, particularly in the coronal plane. However, medicine was being swept away in the tide of drug-based medicine that continues today, and healthcare has largely forgotten his advice. Today, the chiropractic profession champions Goldthwait’s postural advice.
In contrast to the straight-on front and back views of the spinal column, when the spine is viewed from the side, optimum health and function requires four distinct spinal curves (2):
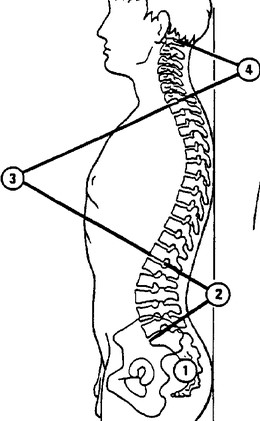
- Sacral Kyphosis
- Lumbar Lordosis
- Kyphosis
- Cervical Lordosis
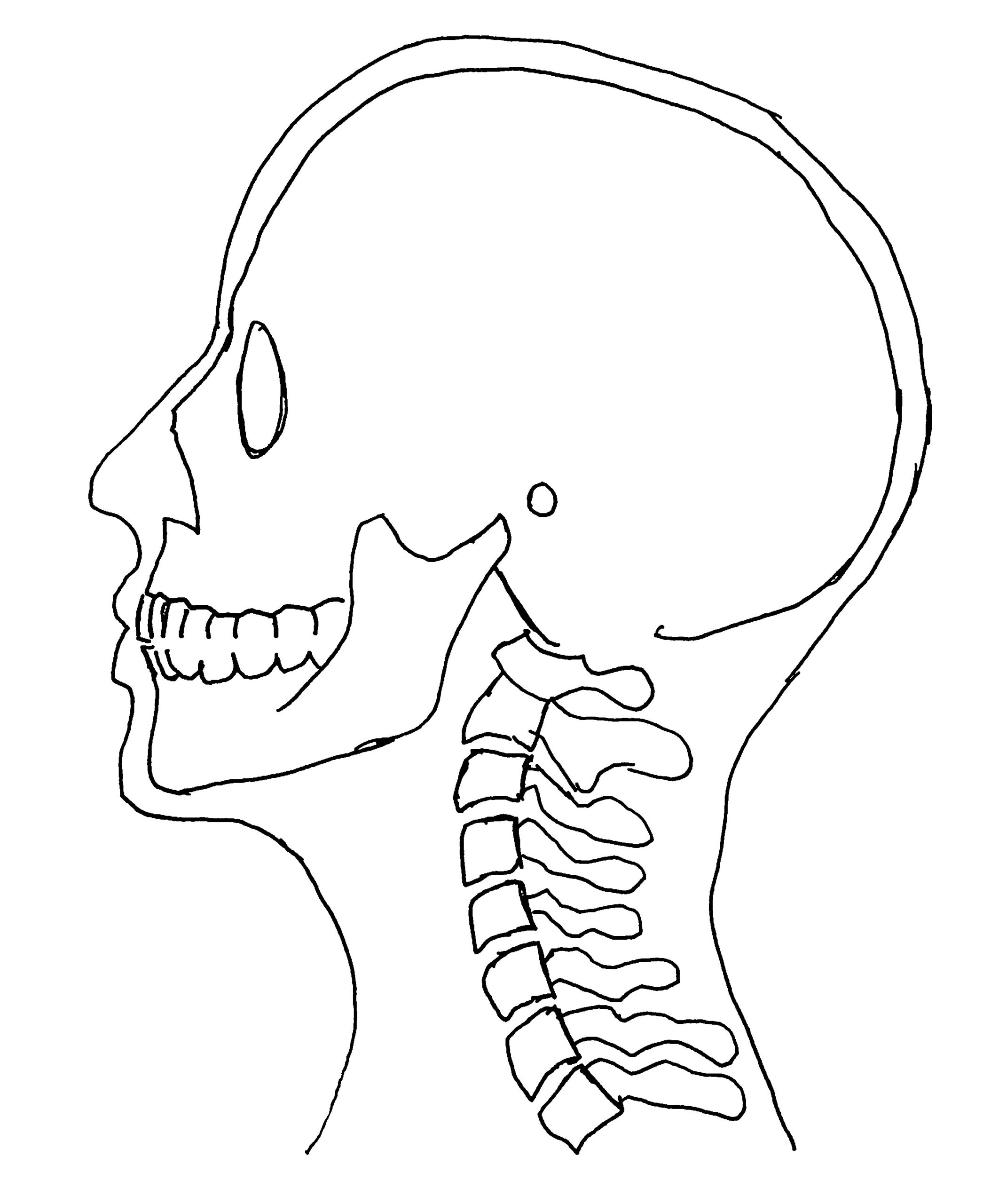
This paper reviews the clinical importance of cervical lordosis.
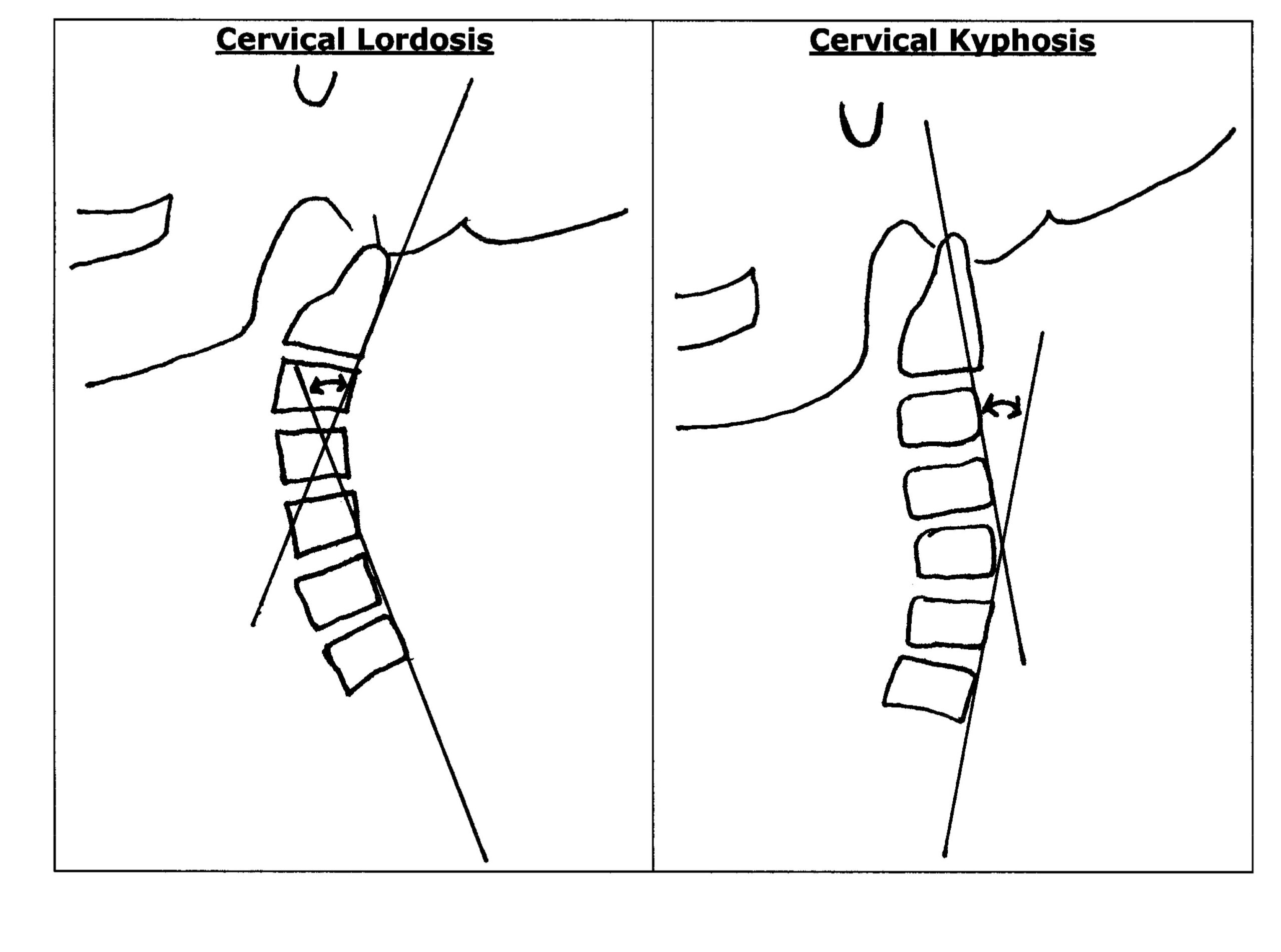
Loss of cervical lordosis is categorized into three groups:
- Hypolordosis: loss of the optimum curvature, but still lordotic.
- Military: complete loss of lordosis resulting in a straight spine.
- Kyphosis: a reversal of the normal lordotic curvature.
Loss of the normal cervical spine lordosis is associated with a number of neuromusculoskeletal problems. The primary problems fall into five categories:
- Lever Arm Stress and the consequent Myofascial Pain Syndromes
- Acceleration of Degenerative Joint Disease
- Spinal Cord Tethering
- Spinal Cord Demyelination
- Vertebral Artery blood flow compromise
Lever Arm Stress and the consequent Myofascial Pain Syndromes
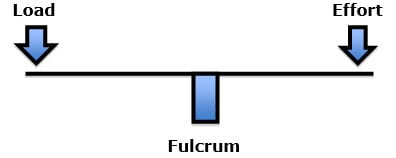
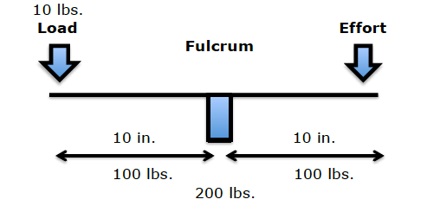
Holding the head up is a first-class lever arm mechanical system. In a first-class lever, the fulcrum is in between the load and the effort. Examples of a first-class lever include a teeter-totter or crowbar:
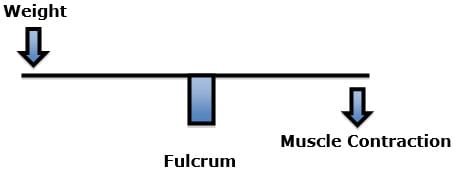
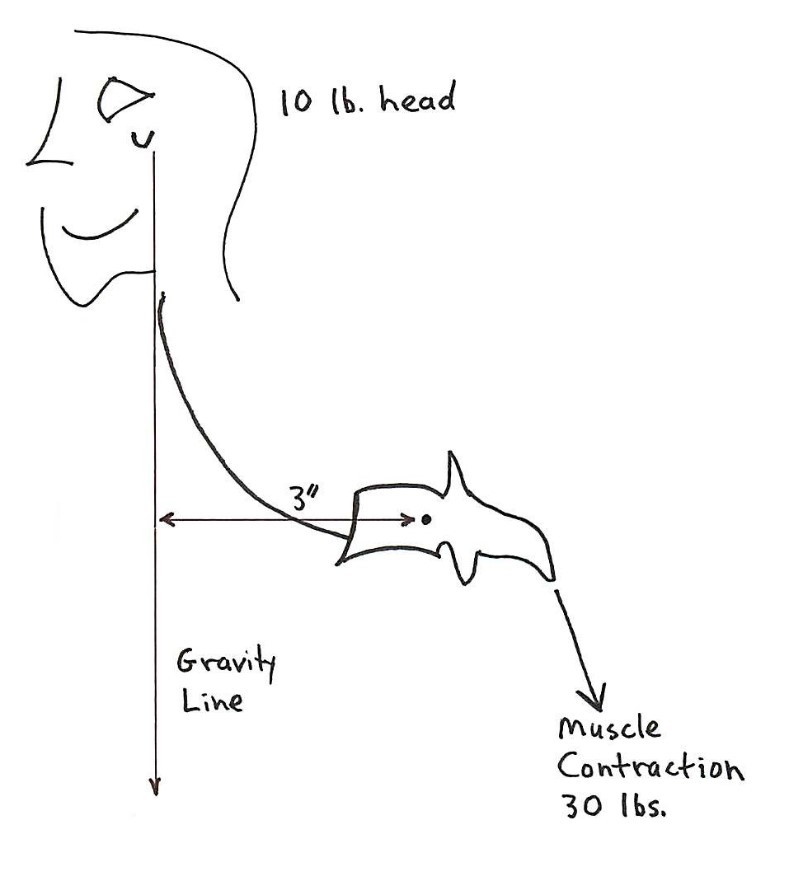
With loss of cervical lordosis, the head and its weight are displaced forward of the spinal column. To prevent such a person from falling onto their face, the muscles in the back of the spinal column will contract to maintain balance (3). The chronic counterbalancing muscle contraction results in chronic inflammation, pain, muscle tissue fibrosis, and functional disability (3). The syndrome associated with this sequence of events has been termed myofascial pain syndrome (4, 5, 6).
If the weight of the head is 10 lbs. and the loss of lordosis displaces the head’s center of gravity forward by 3 inches, the required counter balancing muscle contraction on the opposite side of the fulcrum (the vertebrae) would be 30 lbs. (10 lbs. X 3 inches):
In such cases, muscle therapy (massage and various forms of interventional modalities) is helpful, but not a long-term solution. The best solution is improvement of cervical lordosis, reducing lever-arm stress, allowing the counterbalancing muscles to relax.
Acceleration of Degenerative Joint Disease
As noted above, holding the head up is a first-class lever arm mechanical system. In a first-class lever, the fulcrum is in between the load and the effort. The fulcrum of a first-class lever is the place where the load is the greatest. In the spine, the fulcrum of the first-class lever of upright posture is primarily the vertebral body/disc, and the two facet joints.
Loss of cervical lordosis not only displaces the head forward resulting in counterbalancing muscle contraction, it also significantly increases the load on the fulcrum (the intervertebral disc and facet joints) (7, 8). This causes and accelerates degenerative disc and joint disease in the cervical spine (9, 10).
The acceleration of degenerative disc and joint disease is most pronounced when there is a reversal of the cervical lordosis (kyphosis) (11, 12).
Spinal Cord Tethering
With loss of cervical lordosis there is an elongation (stretching) of the spinal cord (7). Chronic elongation, or tethering, of the spinal cord can result in both spine neuron dysfunction and/or spinal cord vascular compromise (13, 14). These can result in both autonomic and musculoskeletal symptoms.
Spinal Cord Demyelination
An important experimental study was published in the journal Spine in 2005 pertaining to cervical spine kyphosis and demyelination of the spinal cord (15). The article was titled:
Spinal Kyphosis Causes Demyelination and Neuronal Loss
in the Spinal Cord: A New Model of Kyphotic Deformity
This study showed that cervical spine kyphosis resulted in compression of the anterior vascular supplies to the spinal cord, eventually resulting in spinal cord demyelination. The demyelination was greatest at the apex of the kyphotic deformity. Angiography showed a reduction in the density of capillary networks and interruption of capillaries at the compressed spinal cord from kyphosis. The authors state:
“Demyelination of the compressed white matter due to kyphotic deformity progressed in the order of anterior, lateral, and posterior funiculus; the posterior funiculus tended to be preserved even in the cases of severe compression.”
“The anterior funiculus in the [kyphotic] group, was the most extensively compressed, showed most marked histologic changes such as demyelination and irregularity of the spared myelin sheath.”
“As the kyphotic angle increased, these changes became more marked, especially in the ventral side of the spinal cord that was directly exposed to mechanical compression.”
“As kyphosis progressed further, the demyelination of the axon spread to the lateral funiculus and then to the posterior funiculus. Marked histologic changes were seen on the ventral side of the spinal cord, probably because of continuous mechanical stress caused by the kyphotic deformity.”
“Demyelination of the axons progressed in the order of the anterior, lateral, and then posterior funiculus.”
Cervical Axial View
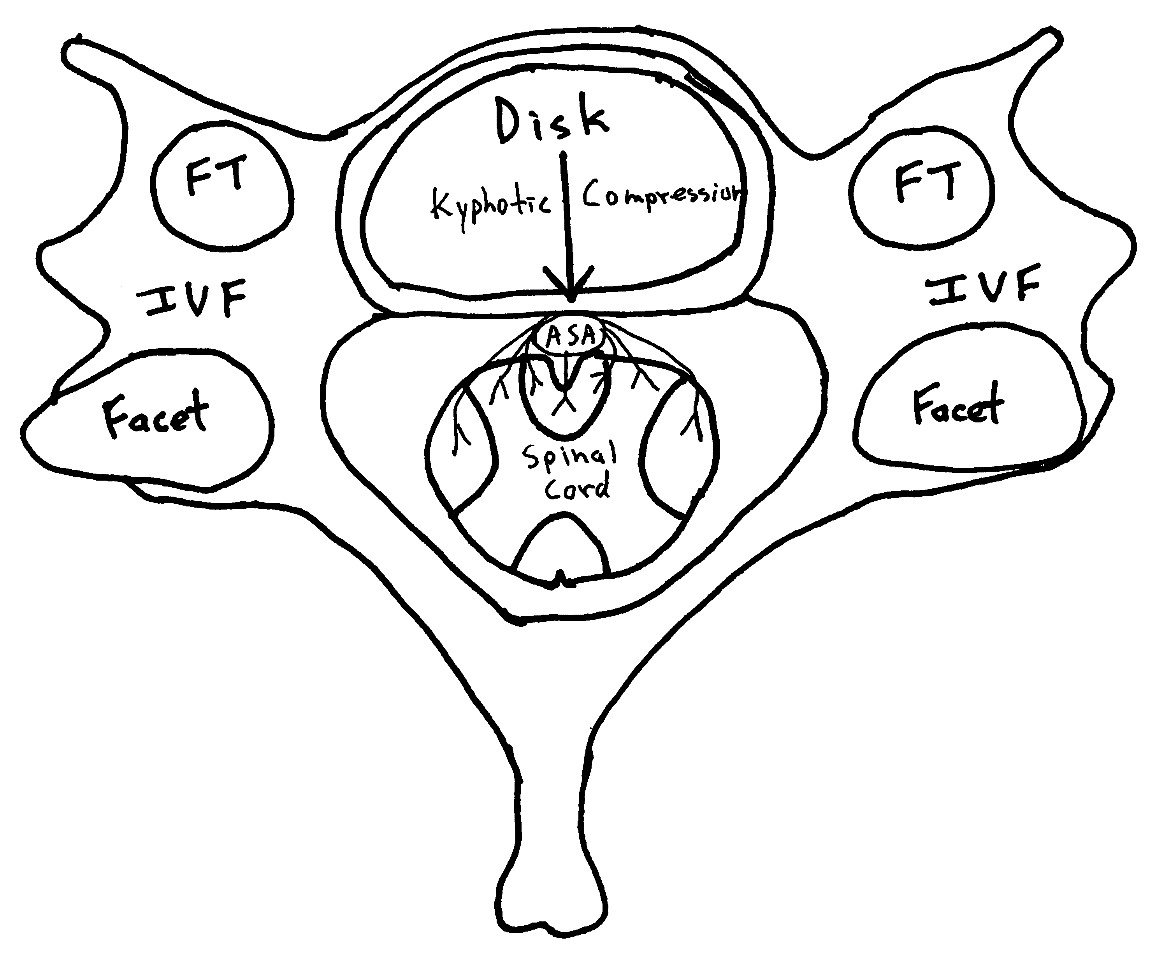
ASA = Anterior Spinal Artery
FT=Foramen Transversarium (where the vertebral artery resides)
IVF=Intervertebral Foramen (where the nerve root resides)
The Anterior Spinal Artery (ASA) is the primary blood supply to the neurons of the anterior and lateral spinal cord.
Cervical Kyphosis cantilevers the anterior spinal cord around the posterior intervertebral disk and vertebral bodies.
Between the posterior intervertebral disk and the anterior spinal cord resides the Anterior Spinal Artery. Cervical kyphosis compresses the Anterior Spinal Artery resulting in ischemia, first to the anterior spinal cord, and later to the lateral spinal cord, causing dysfunction and eventual spinal cord demyelination.
Vertebral Artery Blood Flow Compromise
The vertebral artery is the pipeline carrying blood, nutrients and oxygen to the brainstem. The vertebral artery resides inside the cervical spine vertebrae in an opening termed the foramen transversarium. There is evidence that loss of cervical lordosis results in a compromise of blood flow from the heart, through the vertebral artery in the foramen transversarium and into the brain stem. This would adversely affect cranial nerve and other vital function.
An important article on this topic was published in the journal Medical Science Monitor in 2016, and titled (16):
Decreased Vertebral Artery Hemodynamics in Patients with Loss of Cervical Lordosis
This is the first study to focus on the status of the vertebral artery in patients with loss of cervical lordosis. The authors evaluated the values of the vertebral arteries in patients with loss of cervical lordosis compared to strictly matched control subjects without loss of cervical lordosis.
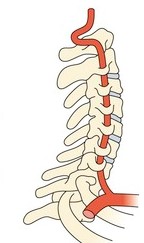
Thirty patients with loss of cervical lordosis and 30 carefully matched controls were assessed bilaterally (60 arteries each group) with Doppler ultrasonography. Vertebral artery hemodynamics, including lumen diameter, flow volume, peak systolic velocity was measured, and values were statistically compared between the patient and the control groups. The cervical lordosis was assessed on lateral cervical radiographs using the posterior tangent method; the lordosis was defined as the angle between the posterior margins of the vertebral bodies C2 and C7. These authors make these points:
“This natural lordotic curvature of the cervical spine is considered to be an ideal posture in terms of biomechanical principles.”
“The normal cervical spine has a lordotic curve. Abnormalities of this natural curvature, such as loss of cervical lordosis or cervical kyphosis, are associated with pain, disability, and poor health-related quality of life.”
“Loss of cervical lordosis causes disrupted biomechanics, triggering a degenerative process in the cervical spine.”
“The present study revealed a significant association between loss of cervical lordosis and decreased vertebral artery hemodynamics, including diameter, flow volume, and peak systolic velocity.”
When the cervical curve flattens, the vertebral arteries “are also in danger of being stretched or compressed.”
“The results of this study indicate that loss of cervical lordosis is associated with decreased vertebral artery values in lumen diameter, flow volume, and peak systolic velocity.”
This article increases the awareness of the adverseness of loss of cervical lordosis. It also highlights the importance of improving and/or correcting cervical lordosis.
••••••••••
Chiropractic clinical practice includes the assessment and treatment of both alignment and the normal lateral spinal curves, including cervical lordosis. The most accurate assessment of spinal curves is with x-rays.
Chiropractors use a number of techniques to improve and/or restore the cervical spine lordosis. There are several studies in the PubMed Database indicating that chiropractic can improve and even reverse cervical kyphosis. The procedures usually involve combinations of certain adjustments and extension traction (17, 18, 19, 20, 21, 22, 23, 24, 25).
REFERENCES:
- Oschman J; Energy Medicine, The Scientific Basis; Chruchill Livingstone; 2000.
- Kapandji IA; The Physiology of the Joints; Volume Three, The Trunk and the Vertebral Column; Churchill Livingstone; 1974.
- Cailliet R; Soft Tissue Pain and Disability; 3rd Edition; FA Davis Company; 1996.
- Travell J, Simons D; Myofascial pain and dysfunction, the trigger point manual; New York: Williams & Wilkins, 1983.
- Travell J, Simons D; Myofascial pain and dysfunction, the trigger point manual: THE LOWER EXTREMITIES; New York: Williams & Wilkins, 1992.
- Simons D, Travell J; Travell & Simons’, Myofascial pain and dysfunction, the trigger point manual: Volume 1, Upper Half of Body; Baltimore: Williams & Wilkins, 1999.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine, Second Edition; Lippincott; 1990.
- Cailliet R; Low Back Pain Syndrome, 4th edition; FA Davis Company; 1981.
- Garstang SV, Stitik SP; Osteoarthritis; Epidemiology, Risk Factors, and Pathophysiology; American Journal of Physical Medicine and Rehabilitation; November 2006; Vol. 85, No. 11; pp. S2-S11.
- Ruch W; Atlas of Common Subluxations of the Human Spine and Pelvis, Second Edition; Life West Press; 2014.
- Uchida K, Nakajima H, Sato R, Yayama T, Mwaka ES, Kobayashi S, Baba H; Cervical Spondylotic Myelopathy Associated with Kyphosis or Sagittal Sigmoid Alignment: Outcome after Anterior or Posterior Decompression; Journal of Neurosurgery: Spine; November 2009; Vol. 11; pp. 521-528.
- Grosso M, Hwang R, Mroz T, Benzel, Steinmetz M; Relationship between degree of focal kyphosis correction and neurological outcomes for patients undergoing cervical deformity correction surgery; Journal of Neurosurgery: Spine; June 18, 2013; Vol. 18; No. 6; pp. 537-544.
- Breig A; Adverse Mechanical Tension in the Central Nervous System; Almqvist and Wiksell; 1978.
- Wing PC, Tsang IK, Susak L, Gagnon F, Gagnon R, Potts JE; Back Pain and Spinal Changes in Microgravity; Orthopedic Clinics of North America; April 1991; Vol. 22; No. 2; pp. 255-262.
- Shimizu K, Nakamura M, Nishikawa Y, Hijikata S, Chiba K, Toyama Y; Spinal Kyphosis Causes Demyelination and Neuronal Loss in the Spinal Cord: A New Model of Kyphotic Deformity; Spine; November 2005; Vol. 30; No. 21; pp. 2388-2392.
- Bulut MD, Alpayci M, Şenkoy E, Bora A, Yazmalar L, Yavuz A, Gulşen I; Decreased Vertebral Artery Hemodynamics in Patients with Loss of Cervical Lordosis; Medical Science Monitor; February 15, 2016; Vol. 22; pp. 495-500
- Leach RA. An evaluation of the effect of chiropractic manipulative therapy on hypolordosis of the cervical spine. J Manipulative Physiol Ther. 1983 Mar;6(1):17-23.
- Harrison DD, Jackson BL, Troyanovich S, Robertson G, de George D, Barker WF. The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study. Journal of Manipulative and Physiological Therapeutics; September 1994; Vol. 17; No. 7; pp. 454-64.
- Troyanovich SJ, Harrison DE, Harrison DD. Structural rehabilitation of the spine and posture: rationale for treatment beyond the resolution of symptoms. J Manipulative Physiol Ther. 1998 Jan;21(1):37-50.
- Harrison DE, Harrison, DD, Haas JW. CBP Structural Rehabilitation of the Cervical Spine, 2002.
- Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: a nonrandomized clinical controlled trial. Arch Phys Med Rehabil. 2002 Apr;83(4):447-53.
- Morningstar MW, Strauchman MN, Weeks DA. Spinal manipulation and anterior headweighting for the correction of forward head posture and cervical hypolordosis: A pilot study. J Chiropr Med. 2003 Spring;2(2):51-4.
- Harrison DE, Harrison DD, Betz JJ, Janik TJ, Holland B, Colloca CJ, Haas JW. Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial. J Manipulative Physiol Ther. 2003 Mar-Apr;26(3):139-51.
- Ferrantelli JR, Harrison DE, Harrison DD, Stewart D. Conservative treatment of a patient with previously unresponsive whiplash-associated disorders using clinical biomechanics of posture rehabilitation methods. J Manipulative Physiol Ther. 2005 Mar-Apr;28(3):e1-8.
- Oakley PA, Harrison DD, Harrison DE, Haas JW. Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. J Can Chiropr Assoc. 200
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

