Posture is important to health and physiology. Entire medical texts and chapters in medical texts are dedicated to posture and its influences (1,2). An excellent description of the importance of gravity and posture on physiology is found in the text by James Oschman, PhD, titled (Oschman):
Energy Medicine, The Scientific Basis
Dr. Oschman notes:
Gravity is the most potent physical influence in any human life. “Gravity pervades our bodies and our environment and affects our every activity. All of the structures around us – our homes, furniture, buildings, machinery, plant, and animal, – and our own bodies, are designed to function in a world dominated by gravity.”
“To introduce the therapeutic significance of gravity, we summarize the work of Joel E. Goldthwait and his colleagues at Harvard Medical School.” “A surgeon in Boston and founder of the orthopaedic clinic at the General Hospital, Goldthwait developed a successful therapeutic approach to chronic disorders. The aim of his therapies was to get his patients to sit, stand, and move with their bodies in a more appropriate relationship with the vertical. After years of treating patients with chronic problems, he concluded that many of these problems arise because parts of the body become misaligned with respect to the vertical, and organ functions therefore become compromised.”
“Goldthwait’s therapeutic approach was based in part on observations made while performing surgery on such patients. He noticed that abdominal nerves and blood vessels are under tension in individuals whose bodies are out of alignment. He also reported ‘stretching and kinking’ of the cerebral arteries and veins in those whose necks were bent. Various cardiac problems were correlated with ‘faulty body mechanics’ that distorted the chest cavity in a way that impaired circulatory efficiency. Goldthwait also documented with X-rays a build-up of calcium deposits around the vertebrae of individuals with chronic arthritis, and observed that these deposits can diminish when the individual acquires a more vertical stance. His therapeutic approach corrected many difficult problems without the use of drugs. He viewed the human body from a mechanical engineering perspective, in which alignment of parts is essential to reduce wear and stress. He pleaded with physicians to recognize and correct misalignments to prevent long-term harmful effects.”
“The basic principle of gravitational biology is known to any child who plays with blocks. The center of gravity of each block must be vertically above the center of gravity of the one below, to have a stable, balanced arrangement. If the center of gravity of one block lies outside of the gravity line, stability is compromised.”
“Likewise, there is only one stable, strain-free arrangement of the parts of the human body. Any variation from this orientation will require corresponding compensations in other parts of the support system.”
“Misalignment of any part will affect the whole system, and that restoration of verticality is a way to address a wide variety of clinical problems.”
Dr. Goldthwait pleaded for everyone to pay more attention to the ways they hold and move their bodies in relation to the gravity field. However, medicine was being swept away in the tide of drug-based medicine that continues today.
••••
Upright posture is a first-class lever mechanical system, such as a teeter-totter or seesaw (4, 5). Increased weight on one side of the fulcrum requires a proportionate contraction of the muscles on the opposite side of the fulcrum in order to maintain upright posture. This counterbalance contraction of the muscles is both fatiguing to the muscle and increases the compressive loads on the fulcrum tissues.
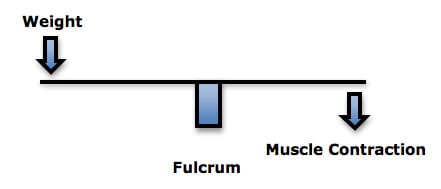
As an example, Rene Cailliet, MD, uses an example where a patient has unbalanced forward head posture (6). Dr. Cailliet assigns the head a weight of 10 lbs. and displaces the head’s center of gravity forward by 3 inches. The required counter balancing muscle contraction on the opposite side of the fulcrum (the vertebrae) would be 30 lbs. (10 lbs. X 3 inches):
The fulcrum of a first class lever is the place where the force is the greatest. In the spine, the fulcrum of the first class lever is the vertebra. Approximately 60% of weight is born by the vertebral body/intervertebral disc complex, and the other 40% is shared between the two facet joints. This means that when the first class lever of upright posture is altered, for any reason, there is an increased mechanical load born by the fulcrum, i.e. the spinal intervertebral discs and facet joints. Such increased mechanical loads accelerate degenerative joint disease (4, 7). In their 1990 book Clinical Biomechanics of the Spine (5), White and Panjabi state:
“The load on the discs is a combined result of the object weight, the upper body weight, the back muscle forces, and their respective lever arms to the disc center.”
The constant muscle contraction required to balance postural distortions creates muscle fatigue and myofascial pain syndromes. Rene Cailliet, MD states “This increase [in muscle tension] not only is fatiguing, but acts as a compressive force on the soft tissues, including the disk.” (4).
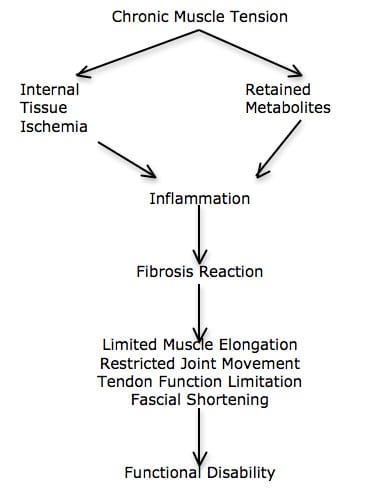
Dr. Cailliet explains how the constant contraction in the counterbalancing muscles creates a cascade that leads to muscle fatigue, inflammation, fibrosis, and eventually to chronic musculoskeletal pain syndromes (6):
••••
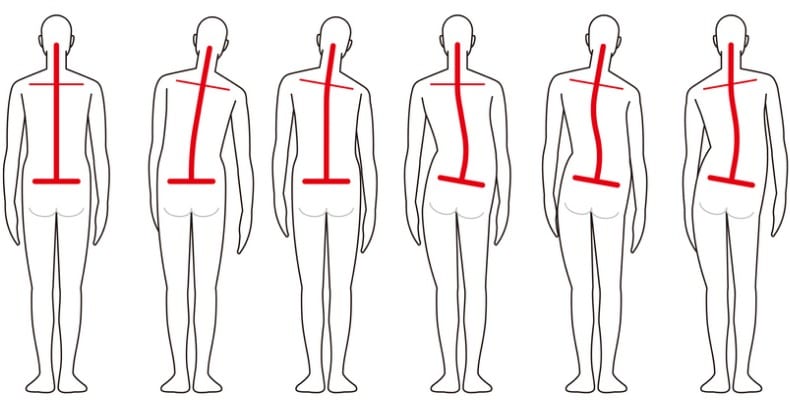
Chiropractors view postural distortions as significantly adversely impacting a patient’s physiology. In the journal Forensic Science International, German physician LE Koch (8) and colleagues suggest that people should have chiropractic treatment if they have “asymmetries in the horizontal and sagittal plane of body posture and motion.”
A number of recent studies have added to the evidence of the deleterious nature of postural distortions. I have reviewed a few of them below.
••••
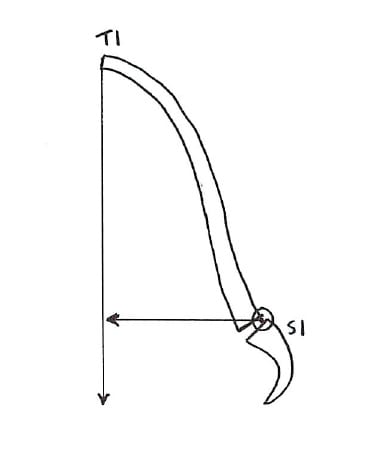
Cervical Lordosis / KyphosisIn 1978, Swedish neurosurgeon Alf Breig, MD authored a book (9) titled Adverse Mechanical Tension in the Central Nervous System. In this book, based upon his own surgical observations, Dr. Breig asserts that loss of cervical lordosis tethers the spinal cord. The spinal cord becomes ischemic and dysfunctional, affecting motor, sensory, and autonomic neurons. Dr. Breig demonstrated that cervical kyphosis produces flattening of the small feeding vessels to the spinal cord. “If the kyphotic deformity continues, there may be progression of myelomalacia and spinal cord atrophy. Patients with long-standing kyphotic deformities are at risk for progression of myelopathy with resultant permanent damage to the spinal cord.”
••••
In 2009, researchers from the Department of Orthopaedics and Rehabilitation Medicine, Fukui University, Japan, published a study in the Journal of Neurosurgery: Spine titled (10):
Cervical Spondylotic Myelopathy Associated with Kyphosis or Sagittal Sigmoid Alignment
These authors assessed the records of 476 patients to determine the effects of kyphotic sagittal alignment of the cervical spine in terms of neurological morbidity. They specifically looked at the effects of sagittal kyphotic deformities or mechanical stress on the development of cervical spondylotic myelopathy.
These authors concluded that cervical spine kyphotic deformity and mechanical stress may play an important role in neurological dysfunction. This was especially true when the kyphotic deformity exceeded 10 degrees. They state:
“In patients with kyphotic deformities, the spinal cord shifts to the anterior portion of the spinal canal and abuts the posterior aspect of the vertebral bodies at the apex of the deformity. With the progression of kyphosis, the mechanical stress applied to the anterior aspect of the spinal cord eventually increases.”
Importantly, 65.1% of the patients showed signs of spinal cord pathology at and around the level of the maximal kyphosis. This was best ascertained with the T2-weighted MRI image. These authors cite references and propose that cervical spine kyphosis distracts (tethers) the spinal cord, and the effects on the cord are maximal at the kyphotic apex, usually C4 and C5 levels. This causes disappearance of spinal cord evoked potentials in that area, causing injury to the anterior horn and the pyramidal tracts (both are muscle motor function). The authors state:
“Loss of lordosis or kyphotic alignment of the cervical spine and spinal cord may contribute to the development of myelopathy, and in patients with cervical kyphotic deformity, the spinal cord could be compressed by tethering over the apical vertebra or intervertebral disc.”
“We conclude that the [cervical spine] sagittal kyphotic deformity related to flexion mechanical stress may be a significant factor in the development of cervical spondylotic myelopathy.”
This article emphasizes the adverseness of cervical spine postural kyphosis: accelerated spondylosis, spinal cord tethering and myelopathy.
••••
In April of this year (2013), another article was published in the Journal of Neurosurgery: Spine, titled (11):
Relationship between degree of focal kyphosis correction and neurological outcomes for patients undergoing cervical deformity correction surgery
These authors performed a retrospective review of 36 patients with myelopathic symptoms who underwent cervical deformity correction surgery. They note:
“The normal lordotic curvature of the cervical spine is critical to maintaining sagittal alignment and spinal balance.”
“It is believed that the neurological symptoms seen in cervical kyphosis are a result of deformity-induced anatomical changes that apply pressure to the spinal cord and nerve roots.”
“The reversal of normal cervical curvature, as seen in kyphosis, can occur through a variety of mechanisms and can lead to mechanical pain, neurological dysfunction, and functional disabilities.”
“Kyphosis of the cervical spine can be a debilitating condition that leads to significant neurological dysfunction.”
“Our study found that the degree of correction of focal kyphosis deformity correlates with improved neurological outcomes.”
It is thought that the tension created from kyphotic deformity on the anterior spinal cord “results in compression on the regional blood supply and nerves.” The results of this study showed significantly improved neurological outcomes with better correction of focal kyphosis and with attainment of global lordosis.
Although this is a surgical study, it has a number of chiropractic applications. Cervical kyphosis adversely affects spinal cord function, probably by contributing to anterior spinal cord ischemia and pressure on the spinal cord and nerve roots. Cervical kyphosis can cause mechanical pain, neurological dysfunction, and functional disabilities. Correction of cervical lordosis is desirable. The better the correction of focal cervical kyphosis and the better the achievement of global cervical lordosis, the better the improvement of neurological outcomes.
••••
Thoracic Kyphosis
The champion of the influence of the thoracic spine posture on health and physiology is physician Deborah Kado, MD. In 2004, Dr. Kado and colleagues published a study in the Journal of the American Geriatrics Society, titled (12):
Hyperkyphotic Posture Predicts Mortality in Older Community-Dwelling Men and Women: A Prospective Study
Hyperkyphosis, commonly known as the dowager’s hump, is frequently observed in older persons. The objective of these authors was to determine the association between hyperkyphotic thoracic posture and rate of mortality and cause-specific mortality in older persons. It was a prospective cohort study that included 1,353 participants. Kyphotic posture was measured as the number of 1.7-cm blocks that needed to be placed under the participant’s head to achieve a neutral head position when lying supine on a rigid radiology table. Individuals with hyperkyphosis cannot lie flat with their heads touching a flat surface unless they hyperextend their necks. Hyperkyphotic posture was defined as requiring one or more blocks under the occiput to achieve a neutral head position while lying supine.
Study participants were followed for an average of 4.2 years, with mortality and cause of death confirmed using review of death certificates.
Persons with hyperkyphotic posture had a 44% increased rate of mortality.
“Hyperkyphotic posture was specifically associated with an increased rate of death due to atherosclerosis.” These authors note:
“Hyperkyphosis is associated with restrictive pulmonary disease and poor physical function, suggesting that hyperkyphosis might be associated with other adverse health outcomes.”
“With increasing kyphotic posture, there was a trend towards greater mortality.”
“For deaths due to atherosclerosis, participants with hyperkyphotic posture had a significant 2.4 times greater rate of death.”
“These study findings place new importance on the clinical finding of hyperkyphotic posture.”
“It is possible that hyperkyphotic posture reflects an increased rate of physiological aging.”
“The realization that hyperkyphosis is not synonymous with vertebral fractures may lead to interventions specifically targeted at improving posture, possibly resulting in reduced mortality rates.”
Interestingly, hyperkyphosis is generally thought to be due to osteoporosis. However, this study did not support that thinking, Noting that hyperkyphosis is not primarily caused by osteoporosis. The authors note that interventions specifically targeted at improving hyperkyphotic posture could result in reduced mortality rates.
••••
In 2009, Dr. Deborah Kado and colleagues published a follow-up study on thoracic kyphosis and mortality rates. This article appeared in the Annals of Internal Medicine, and is titled (13):
Hyperkyphosis Predicts Mortality Independent of Vertebral
Osteoporosis in Older Women
The objective of this study was to determine whether thoracic hyperkyphosis predicts increased mortality. It was also a prospective cohort study, and it involved 610 women, aged 67 to 93 years. Their thoracic kyphosis was measured, and mortality was assessed an average of 13.5 years later.
The authors concluded that each standard deviation increase in kyphosis carried a 14% increased risk for death.
After adjustment for age and other predictors of mortality, including such osteoporosis-related factors as low bone density, moderate and severe prevalent vertebral fractures, and number of prevalent vertebral fractures, women with greater kyphosis were at increased risk for earlier death by 15%. These authors note:
“In older women with previous vertebral fractures, increased kyphosis predicts increased risk for all-cause mortality independent of the extent and severity of the underlying spinal osteoporosis.”
“Other large epidemiologic studies have demonstrated that kyphotic posture may be associated with worse health, including impaired pulmonary function, poor physical function, inferior quality of life, injurious falls, fractures, and death.”
“Our previous work and that of others demonstrated an association between hyperkyphosis and compromised pulmonary function and pulmonary death.”
“We postulate that the phenotype of hyperkyphosis is an easily assessable clinical marker of accelerated physiologic aging or frailty.”
“Hyperkyphosis may be a good marker of at least 1 category of a frail phenotype.”
“These results add to a growing literature that suggests that hyperkyphosis is a clinically important finding.”
“Because it is readily observed and is associated with ill health in older persons, hyperkyphosis should be recognized as a geriatric syndrome—a ‘multifactorial health condition that occurs when the accumulated effect of impairments in multiple systems renders a person vulnerable to situational challenges.’”
This study reinforces the concept that altered posture affects systemic health, quality of life, and mortality.
••••
Lumbar Kyphosis and the Forward (Anterior) Gravity Line
Two studies have found that when a person has lumbar kyphosis, the entire spinal column is pitched forward. The first study was published by physician Steven Glassman, MD, and colleagues, in the journal Spine in 2005, and titled (14):
The Impact of Positive Sagittal Balance in Adult Spinal Deformity
These authors measured the pain, systemic health, and disability status of 298 individuals and compared such measurements to a radiographic measurement of sagittal postural balance. A full-spine (36 inch) lateral x-ray was exposed. A plum line was dropped from the body of the C7 vertebrae and measured with respects to the articulating surface of L5 with the sacral base. All measures of health status showed significantly poorer scores as C7 plumb line deviation increased in the forward direction (anterior to the sacral base). The authors note:
“Patients with relative kyphosis in the lumbar region had significantly more disability than patients with normal or lordotic lumbar sagittal measures.”
“This study shows that although even mildly positive sagittal balance is somewhat detrimental, severity of symptoms increases in a linear fashion with progressive sagittal imbalance.”
“The results also show that kyphosis is very poorly tolerated in the lumbar spine.”
“There was clear evidence of increased pain and decreased function as the magnitude of positive [forward] sagittal balance increased.”
“All measures of health status showed significantly poorer scores as C7 plumb line deviation increased [forward].”
“This study shows that although even mildly positive [forward] sagittal balance is somewhat detrimental, severity of symptoms increases in a linear fashion with progressive [forward] sagittal imbalance.”
This study is quite supportive of postural chiropractic techniques that stress the importance of the restoration of sagittal balance and restoration of lumbar lordosis.
••••
The second study was published only a few days ago (May 2013). It was published in The Journals of Gerontology: Series A: Biological Sciences, and titled (15):
Spinal Posture in the Sagittal Plane Is Associated With Future Dependence in Activities of Daily Living
These authors noninvasively measured spinal postures in a community-based prospective cohort of older adults (804 participants: 338 men, 466 women, age range 65–94 years) to determine if any such postures were associated with the need for future assistance in Activities of Daily Living (ADL). They found that lumbar kyphosis pitched the body and head forward, and this postural distortion was significantly associated with the need for future assistance in the person’s activity of daily living. Specifically, when comparing postures in quartiles:
Best v. second: 46% increased risk of need for ADL assistance
Best v. third: 290% increased risk of need for ADL assistance
Best v. fourth: 393% increased risk of need for ADL assistance
These authors state:
“Accumulated evidence shows how important spinal posture is for aged populations in maintaining independence in everyday life.”
“Spinal posture changes with age, but accumulated evidence shows that continued good spinal posture is important in allowing the aged to maintain independent lives.”
Larger anterior inclination of the trunk causes a greater decline in balance and gait skills. “Declines in balance and gait skills caused by inclination lead to falls and fractures, and that these negative outcomes in turn lead to dependence in ADL among elderly people.”
“The gravity line moves further anterior as inclination of the trunk increases.” “Even mildly positive sagittal balance is somewhat detrimental, the decline in health status increases in a linear fashion with progressive sagittal imbalance.”
Spinal “inclination is associated with future dependence in ADL among older adults and warrants wider attention.”
The “results indicate that attention needs to be paid to inclination in spinal posture to identify elderly people at high risk of becoming dependent in ADL.”
This article adds to the evidence that sagittal posture is very important in human physiology, pain, health, and predictive of the ability for one to take care of themselves as they age (ADL). The most egregious postural distortion is an anterior inclination. Forward posture is associated with a loss of lumbar lordosis, and this could be a site of therapeutic intervention.
••••
For decades, biomechanically based chiropractors have recognized the adverseness of postural distortions. A number of chiropractic techniques are primarily concerned with assessing, preventing, and changing these (and other) postural distortions. There are several studies in the PubMed Database indicating that chiropractic can improve and even reverse cervical kyphosis. The procedures usually involve combinations of certain adjustments and extension traction.
Postural distortions necessitate constant contraction of the counter-balancing musculature, resulting in fatigue and pain. The long-term consequences includes acceleration of degenerative joint disease as well as spinal cord tethering and increased risk for myelopathy.
Chiropractic groups have researched many methods for improving postural distortions. These methods included certain adjusting methods, exercises, and traction protocols that involve cervical extension. These methods have proven to be successful (16, 17, 18, 19, 20, 21, 22, 23, 24).
References
- Kendall HO, Kendall FP, Boynton DA; Posture and Pain, Williams and Wilkins, 1985.
- Mennell JM; “The Forward Head Syndrome” in The Musculoskeletal System, Differential Diagnosis from Symptoms and Physical Signs; Aspen; 1992.
- Oschman J; Energy Medicine, The Scientific Basis; Chruchill Livingstone; 2000.
- Cailliet R; Low Back Pain Syndrome, 4th edition, F A Davis Company, 1981.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine, Second Edition, Lippincott, 1990.
- Cailliet R; Soft Tissue Pain and Disability; 3rd Edition; F A Davis Company, 1996.
- Garstang SV, Stitik SP; Osteoarthritis; Epidemiology, Risk Factors, and Pathophysiology; American Journal of Physical Medicine and Rehabilitation; November 2006, Vol. 85, No. 11, pp. S2-S11.
- Koch LE, Koch H, Graumann-Brunt S, Stolle D, Ramirez JM, Saternus KS; Heart rate changes in response to mild mechanical irritation of the high cervical spinal cord region in infants; Forensic Science International; Volume 128, Issue 3, August 28, 2002, pp. 168-176.
- Breig A; Adverse Mechanical Tension in the Central Nervous System; Almqvist and Wiksell; 1978.
- Kenzo Uchida, M.D., Ph.D., Hideaki Nakajima, M.D., Ph.D., Ryuichiro Sato, M.D., Ph.D., Takafum i Yayama, M.D., Ph.D., Erisa S. Mwaka, M.D., Shigeru Kobayashi, M.D., Ph.D., and Hisatoshi Baba, M.D., Ph.D. Cervical Spondylotic Myelopathy Associated with Kyphosis or Sagittal Sigmoid Alignment: Outcome after Anterior or Posterior Decompression; Journal of Neurosurgery: Spine; November 2009, Volume 11, pp. 521-528.
- Matthew Grosso, BS; Roy Hwang MD; Thomas Mroz MD; Edward Benzel MD; Michael Steinmetz MD; Relationship between degree of focal kyphosis correction and neurological outcomes for patients undergoing cervical deformity correction surgery; Journal of Neurosurgery: Spine; April 5, 2013 [epub].
- Deborah M. Kado, MD, MS, Mei-Hua Huang, DrPH, Arun S. Karlamangla, MD, PhD, Elizabeth Barrett-Connor, MD and Gail A. Greendale, MD; Hyperkyphotic Posture Predicts Mortality in Older Community-Dwelling Men and Women: A Prospective Study; Journal of the American Geriatrics Society; Volume 52Issue 10Page 1662 – October 2004.
- Deborah M. Kado, MD, MS; Li-Yung Lui, MA, MS; Kristine E. Ensrud, MD; Howard A. Fink, MD, MPH; Arun S. Karlamangla, PhD, MD; Steven R. Cummings, MD; Hyperkyphosis Predicts Mortality Independent of Vertebral Osteoporosis in Older Women; Annals of Internal Medicine; May 19, 2009; Volume 150; Number 10 W-121; pp. 681-687.
- Glassman, Steven D. MD; Bridwell, Keith MD; Dimar, John R. MD; Horton, William MD; Berven, Sigurd MD; Schwab, Frank MD; The Impact of Positive Sagittal Balance in Adult Spinal Deformity; Spine; Volume 30(18), September 15, 2005 pp. 2024-2029.
- K Kamitani, T Michikawa, S Iwasawa, N Eto, T Tanaka, T Takebayashi, Y Nishiwaki; Spinal Posture in the Sagittal Plane Is Associated With Future Dependence in Activities of Daily Living: A Community-Based Cohort Study of Older Adults in Japan; The Journals of Gerontology: Series A: Biological Sciences; May 2013; Vol. 68; No. 5.
- Leach RA. An evaluation of the effect of chiropractic manipulative therapy on hypolordosis of the cervical spine. J Manipulative Physiol Ther. 1983 Mar;6(1):17-23.
- Harrison DD, Jackson BL, Troyanovich S, Robertson G, de George D, Barker WF. The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study.J Manipulative Physiol Ther. 1994 Sep;17(7):454-64.
- Troyanovich SJ, Harrison DE, Harrison DD. Structural rehabilitation of the spine and posture: rationale for treatment beyond the resolution of symptoms. J Manipulative Physiol Ther. 1998 Jan;21(1):37-50.
- Harrison DE, Harrison, DD, Haas JW. CBP Structural Rehabilitation of the Cervical Spine, 2002.
- Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: a nonrandomized clinical controlled trial. Arch Phys Med Rehabil. 2002 Apr;83(4):447-53.
- Morningstar MW, Strauchman MN, Weeks DA. Spinal manipulation and anterior headweighting for the correction of forward head posture and cervical hypolordosis: A pilot study. J Chiropr Med. 2003 Spring;2(2):51-4.
- Harrison DE, Harrison DD, Betz JJ, Janik TJ, Holland B, Colloca CJ, Haas JW. Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial. J Manipulative Physiol Ther. 2003 Mar-Apr;26(3):139-51.
- Ferrantelli JR, Harrison DE, Harrison DD, Stewart D. Conservative treatment of a patient with previously unresponsive whiplash-associated disorders using clinical biomechanics of posture rehabilitation methods. J Manipulative Physiol Ther. 2005 Mar-Apr;28(3):e1-8.
- Oakley PA, Harrison DD, Harrison DE, Haas JW. Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. J Can Chiropr Assoc. 200
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.