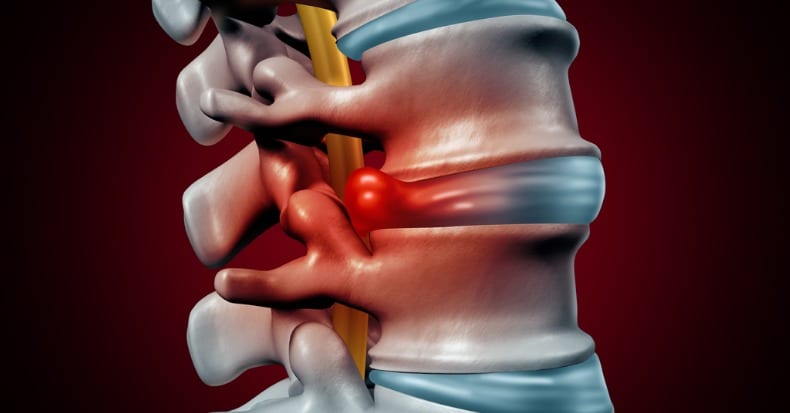
It stands to reason the more an intervertebral disk herniates, the more it will compress the spinal nerves, leading to a greater likelihood for surgical intervention. But what if that isn’t the case?
The current standard treatment of lumbar disk herniation (LDH) involves FIRST the initial use of non-surgical care for at least six weeks. If that fails, a surgical consult can be considered. Exceptions to this rule include the presence of a red flag or a dangerous, potentially life-altering or life-ending condition like infection, fracture (unstable), cancer, and/or cauda equina syndrome (pinched cord altering bowel and bladder control)—all of which are (thankfully) NOT common.
In a study that involved 368 LDH patients who underwent at least six weeks of non-surgical care, researchers observed that 91.3% did not undergo surgery within the following year. A review of MRI findings of the patients who did vs. did not have a surgical procedure showed no difference with respect to what percentage of the spinal canal was inhibited by LDH (31.2% vs. 31.5%). The research team concluded that percentage of canal occluded by LDH does not predict which patients will fail non-surgical care and require surgery.
This finding is important because many spine surgeons still use the size of the lumbar disk herniation to determine if a patient is a candidate for surgery.
While the findings from the previously mentioned study suggest that 9 in 10 LDH patients can avoid surgery, is there any data to indicate which LDH patients might not respond well to surgical care if they do choose that route? A 2019 study investigated this question and reported that the persistence of leg pain may be a key factor. The authors reviewed 556 patient files over a three-year time frame and found that moderate to severe leg pain at early post-surgical follow-up correlated with higher disability scores over time. This group of patients was more likely have both a history of smoking and chronic back pain. This makes some sense as smokers often face a greater risk for post-surgical complications (many surgeons won’t operate on smokers if they can avoid it) and a history of chronic back pain suggests other factors may be responsible for the patient’s current pain and disability, not just the LDH.
The good news is that treatment guidelines support chiropractic care as a non-surgical option for the LDH patient through a combination of spinal manipulation, mobilization, specific exercises, modalities, and nutritional recommendations.
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.