Chiropractic Analysis
and Management
For decades, chiropractic and spinal manipulation has proven to be very effective for the management of low back pain (1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17). Yet, chiropractic does not fix or improve all patients. Some patient’s problems are more complex making their case more difficult. The objective of this presentation is to share some of the critical thinking and clinical management for stubborn cases of low back pain.
Studies indicate that chronic low back pain is primarily discogenic (18, 19, 20, 21). It is also understood that the intervertebral disc is particularly intolerant to rotational stress (22).
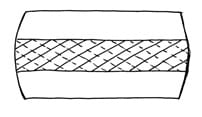
The fibers of the annulus (outer portion) of the intervertebral disc are arranged in layers, and each layer is crossed in opposite directions. During chronic rotational stress on the disc, half of the annular fibers become tense, and the other half become lax. Since rotational stress applied to the annulus is resisted by only half of the annular fibers, the disc is operating at only half strength. This increases the vulnerability of the disc to injury and degenerative disease.
Crossed Annular Fibers of the Intervertebral Disc
An appropriate clinical question pertaining to a patient with stubborn chronic back pain is:
“Is there a chronic rotational stress on a low back disc that may be causing the chronic pain?”
A common differential assessment of such a patient would include evaluation for a clinically relevant “short leg syndrome,” because the short leg syndrome causes a chronic rotational stress on the low back intervertebral discs (23).
In a study by Ora Friberg (23), standing radiographs of the pelvis and lumbar spine in 288 consecutive patients with chronic low back pain and in 366 asymptomatic controls were exposed. His findings showed that 73% of the subjects assessed had meaningful inequality of a lower limb (>5 mm shortness). The incidence of leg length inequality in LBP patients was significantly higher than in asymptomatic controls (more than twice as much).
Friberg emphasized the counter-rotational stresses on the L5-S1 disc:
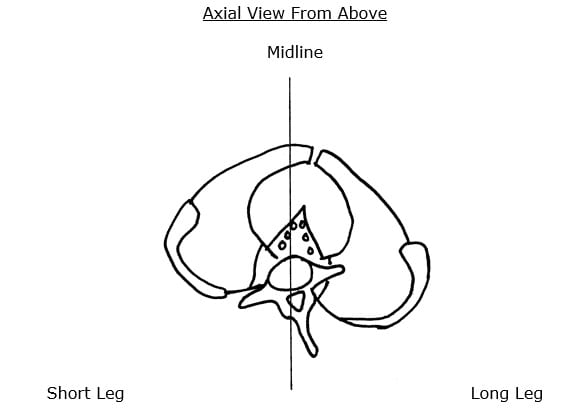
-
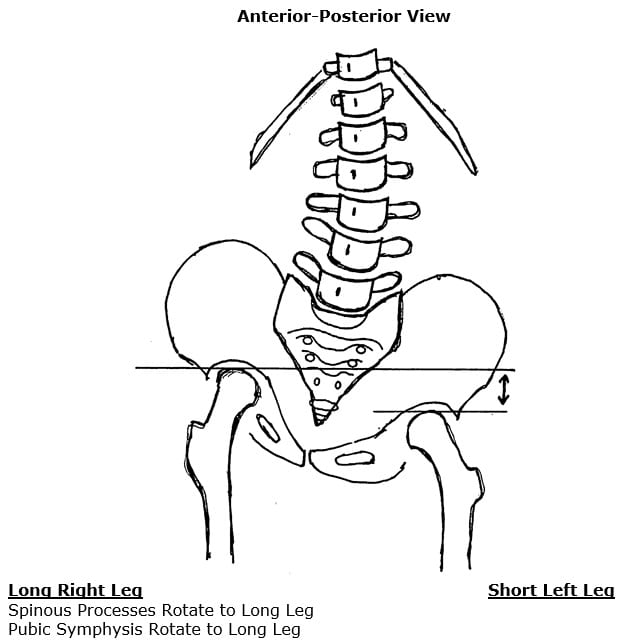
- The L5 spinous process will rotate to the right of midline, towards the side of the long leg. This causes a counterclockwise rotation of the L5-S1 intervertebral disc.
- The pubic symphysis and pelvis will also rotate to the right of midline, also towards the side of the long leg. Because the pubic symphysis is in the anterior, this causes a clockwise rotation of the pelvis and sacrum, and a clockwise rotation of the L5-S1 intervertebral disc.
- This results in “significant” counter-rotational stresses, primarily at the L5-S1 intervertebral disc. The consequences of these counter-rotational stresses at the L5 disc are accelerated disc degeneration and degradation, back pain and sciatica.
••••••••••
Levers
Pisa is a town in Italy. Pisa is notorious for its “Leaning Tower.” Groundbreaking for the Leaning Tower of Pisa was in the year 1173, and it was completed in 1372. The angle of the lean was 4 degrees and increasing over the centuries, putting the tower at risk of falling over. Modern technology and efforts have reduced the lean and hence have reduced the risk of falling over. The Leaning Tower of Pisa is solely mechanical (as opposed to biomechanical).
When humans lean, in any direction, and at angles much greater than 4 degrees, they do not fall over. This is because humans are biomechanical. When humans lean, our muscles contract in a manner to counter-balance the lean, keeping us upright (24, 25). Humans are capable of doing this because upright human posture is a first-class lever mechanical system (24, 25).
In the first-class lever, the fulcrum is between the load and the effort. The fulcrum of a first-class lever is the place where the load is the greatest. In humans, the fulcrum is the weight-bearing portions of the spinal column, which includes the intervertebral disc
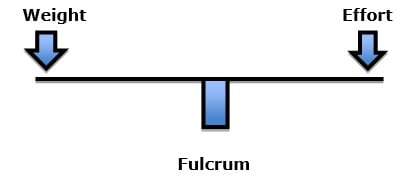
Examples of a first-class lever include a teeter-totter or crowbar.
The load experienced at the fulcrum (spine/disc) of a first-class lever system is dependent upon three factors:
-
- The magnitude of the weight
- The distance the weight is away from the fulcrum (lever arm)
- The addition of the counterbalancing effort required to remain balanced
In humans, the greater the postural distortion (lean), the greater the load on the weight-bearing spine (fulcrum/disc) and the greater the required counter-balancing muscle contraction (effort) to maintain upright posture.
•••••
In his book Energy Medicine, The Scientific Basis, James Oschman, PhD, notes that gravity is the most potent physical influence in any human life (26). He states:
“The basic principle of gravitational biology is known to any child who plays with blocks. The center of gravity of each block must be vertically above the center of gravity of the one below, to have a stable, balanced arrangement. If the center of gravity of one block lies outside of the gravity line, stability is compromised.”
“There is only one stable, strain-free arrangement of the parts of the human body. Any variation from this orientation will require corresponding compensations in other parts of the support system. Misalignment of any part will affect the whole system.”
•••••
In her book Move Your DNA: Restore Your Health Through Natural Movement, biomechanist Katy Bowman, in agreement with Dr. Oschman, notes “Gravity is one force your body responds to constantly.” (27) Ms. Bowman clearly explains the difference between weight and load, emphasizing that the real problem is the load, which is the weight multiplied by a lever distance from a fulcrum, and of course adding the counter-balancing efforts of muscles. She states:
“The loads created by gravity depend upon our physical position relative to the gravitational force.”
The load created by gravity differs depending on alignment with the “perpendicular force of gravity.”
“Every unique joint configuration, and the way that joint configuration is positioned relative to gravity, and every motion created, and the way that motion was initiated, creates a unique load that in turn creates a very specific pattern of strain in the body.” This is called “load profile.”
“It’s not the weight that breaks you down, it’s the load created by the way you carry it.”
“Loads are often oversimplified to ‘weight’ because it makes them easier to understand, but there is much more going on with your sore knee (or foot, or back, or pelvic floor) than your weight.”
“Weight is not the be-all and end-all of loads. When you want to improve your health, it’s much more important to consider how you carry your weight than to spend hours contemplating the lone data point that is Your Weight.”
Ms. Bowman also emphasizes the importance of time. A temporary change in postural positioning affects the body quite differently than a chronic postural distortion. She states:
“The timing and rates of loads are important because loads are occurrences over a period of time.”
•••••
The Short Leg Syndrome, Postural Distortions,
Chronic Increased Loads, Counter-rotational
Disc Stress, and Low Back Pain
In 1946, Lieutenant Colonel Weaver Rush and Captain Howard Steiner meticulously exposed upright lumbosacral x-rays on 1,000 soldiers for the specific purpose of measuring differences in their leg lengths and to determine if leg length inequality was a factor in the incidence of back pain. They published their results in the American Journal of Roentgenology and Radium Therapy in an article titled (28):
A Study of Lower Extremity Length Inequality
The authors constructed a spinal fixation and stabilization device to ensure the accuracy of upright measurements of leg length and their effects on spinal alignment. The 1,000 soldiers in this study were consecutive, non-selected cases who were sent to the roentgen department because of a low back complaint. The authors concluded, “it is possible to accurately measure differences in lower extremity lengths as manifested by a difference in the heights of the femoral heads.” They noted:
23% of the soldiers had legs of equal length.
77% of the soldiers had unequal length of their legs.
Leg length differences exceeding 5 mm were associated with the greatest low back pain or disability, and therefore 5 mm is labeled as being a “marked difference.” The authors stated:
“For this reason, it is our opinion that the existence of such a condition [a short leg exceeding 5 mm] is significant from the standpoint of symptomatology and disability.”
They also noted that the short leg was associated with a tilt of the pelvis and a scoliosis, stating:
Whenever there is a pelvic tilt, “there exists coincidentally a scoliosis of the lumbar spine.”
“Because this scoliosis, in all instances, compensates for the tilt of the pelvis, it is referred to by us as compensatory scoliosis.”
“The existence of this compensatory scoliosis in the presence of a tilted pelvis due to shortening of one or the other lower extremity is believed by us to have clinical significance.”
“It was a general consistent observation that the degree of scoliosis was proportionate to the degree of pelvic tilt. An individual who has a shortened leg will have to compensate completely if he intends to hold the upper portion of his body erect or in the midsagittal plane.”
“A consistent observation which has been made is that in those cases with a shortened leg there is a corresponding tilt of the pelvis and a compensatory scoliosis of the lumbar spine.”
The short leg creates the “leaning tower.” The compensatory scoliosis is the counter-balance by muscle contraction so that the patient does not fall over. The Problem:
-
- This significantly increases the load at the fulcrum, including the intervertebral disc.
- As noted by Friberg above (23), the disc is subjected to chronic counter-rotational stress.
•••••
Perhaps the best known short leg syndrome and chronic low back pain subject is former US President John F. Kennedy (b. May 29, 1917). President Kennedy’s back problems significantly worsened in August of 1943 during the sinking of his boat PT-109 in the Pacific during WWII. Kennedy’s back problems never fully recovered from that war injury, for which he was awarded the Purple Heart.
In 1954, then Senator Kennedy underwent an attempted spinal fusion operation, and it went badly; it was his second spinal surgery for his persistent low back pain. He nearly died, and his recovery took 8 months. The following year, Kennedy came under the care of myofascial pain expert Janet Travell, MD.
When Dr. Travell first saw Senator Kennedy in May of 1955, he was non-ambulatory. He had suffered from 2 devastating spinal surgeries, yet he continued to suffer from debilitating back spasm and left leg pain. Things were so bad that Senator Kennedy was “questioning his ability to continue his political career.”(29) Dr. Travell treated Senator Kennedy. His improvement was so impressive that Dr. Travell’s daughter wrote (30):
“Senator Kennedy received so much relief of pain from my mother’s medical treatments that he had ‘new hope for a life free from crutches if not from backache’.”
In 2003, James Bagg wrote this, pertaining to Dr. Travell (29):
“Jack Kennedy saw a great many physicians over the course of his short life, but one of them, according to his brother Bobby, enabled Jack to become President of the United States.”
Dr. Travell “discovered that one of [Senator] Kennedy’s legs was shorter than the other and made heel lifts for all of his left shoes to counter that additional source of stress on his back.” “Dr. Travell had a workbench in her office and made lifts for both patients and family members. ‘One of the first things I did for him [Kennedy] was to institute a heel lift—a correction for the difference in leg length’.”(29)
•••••
Over the decades, numerous studies have continued to document the relationship between the anatomical short leg syndrome, pelvic unleveling, and chronic back pain (31, 32, 33, 34, 35, 36, 37, 38, 39).
•••••
A recent (2018) study pertaining to the biomechanical consequences of an anatomical short leg was published in the Journal of Bone and Joint Surgery Reviews and titled (40):
Leg-Length Discrepancy, Functional Scoliosis, and Low Back Pain
The authors are from the Hospital for Special Surgery, New York. They note that leg-length discrepancy results in a functional scoliosis when the lumbar spine compensates for pelvic obliquity to maintain shoulder balance.
The authors define a functional scoliosis as one that corrects when an appropriate heel lift is placed under the shorter leg:
“When evaluating a patient with leg length discrepancy and scoliosis radiographically, a true functional scoliosis will correct completely or partially when the pelvis is leveled with blocks placed under the short leg.”
They note that in addition to the functional scoliosis, patients with leg length discrepancy also often suffer from lower back pain. They note that the standard evaluation of these patients is radiographic. These radiographs are taken both initially when the leg length discrepancy is posturally suspected, and again after the use of heel lifts to assess correction. They state:
“Patients with leg length discrepancy, low back pain, and functional scoliosis should undergo radiographic evaluation with the pelvis leveled using blocks placed under the shorter limb.”
The authors note, that as a general rule, leg length discrepancy patients are managed with the use of a “shoe lift,” but if the discrepancy exceeds 20 mm (slightly more than ¾ inch), a surgical correction may be necessary.
Leg length discrepancy cause asymmetries of weight-bearing. In children, asymmetries of weight-bearing adversely affect the growth plates of the weight-bearing bones, especially the legs and the spinal vertebra. This means that leg length discrepancies tend to become greater with growth and age (41). However, in children, these growth asymmetries tend to be asymptomatic. Yet, they may be the real cause of adult symptomatology and adult degenerative changes. This would suggest that asymptomatic children should be evaluated for growth asymmetries and correction is advised to reduce incidences of adult biomechanical problems. These authors state:
“While children typically do not complain of low back pain in the setting of leg length discrepancy, the available evidence suggests that long-standing leg length discrepancy may cause permanent changes in lumbar spine biomechanics, predisposing these patients to future low back pain and degenerative scoliosis.”
Long standing leg length discrepancy and asymmetries of weight bearing are associated with acceleration of articular degenerative changes as well as histological and functional changes in the counter-balancing musculature. These authors note the following:
“Pelvic tilt and compensatory, or functional, scoliosis in the short term resulted in asymmetrical loading of the intervertebral discs and facet joints in the lumbar spine.”
“Patients with leg length discrepancy had a significantly increased prevalence of degenerative joint disease at the L5/S1 spinal motion segment and at the L4/L5 segment compared with cohorts without leg length discrepancy.”
“Long-standing leg length discrepancy may result in degenerative changes of the lumbar spine, altered gait mechanics, and low back pain.”
“Long-standing abnormal spinal biomechanics were thought to result in degenerative disc disease and permanent changes in the lumbar spine.”
“Superimposed functional scoliosis is likely to result in accelerated disc degeneration.”
“When L5/S1 segment degeneration was evaluated as a function of age, men >50 years old with leg length discrepancy had a significantly increased prevalence of degenerative changes compared with an age-matched cohort without leg length discrepancy.”
“There is evidence to support leg length discrepancy as a cause of persistent biomechanical changes in the lumbar spine, and those biomechanical abnormalities may result in permanent degenerative changes to the vertebral bodies.”
“Long-duration functional scoliosis may result in permanent biomechanical changes in the lumbar spine.”
“Leg length discrepancy of >10 mm [slightly less than ½ inch] can generate substantial changes in gait, with greater differences in leg length having greater impact.”
These authors note that the best initial approach for the management of patients with leg length discrepancy, symptomatology, and/or disability is the insertion of an appropriate shoe lift. They reference a study in which correction of leg length discrepancy with a shoe lift for 6 months resulted in “91% reported either decreased or resolved symptoms.” They note that the positive response was greatest in those who spent substantial time standing and those with spondylolysis and/or spondylolisthesis.
The authors reference a second study in which a small group (twelve subjects) of patients with low back pain and chronic leg length discrepancy, found that the use of shoe lifts was associated with significant improvement in terms of general pain, pain with standing, and disability.
Low back surgery is commonplace and often disabling (42). These authors suggest that acknowledgement and correction of leg length discrepancy may reduce the incidence of lumbar spine surgery. They state:
“There is a correlation, if not a cause-and-effect relationship, between pelvic obliquity and degenerative scoliosis resulting in lumbar spine surgery.”
SUMMARY
These concepts and studies support a rationale for why all people should be evaluated chiropractically for leg length discrepancy, pelvic asymmetry and functional scoliosis. This is especially appropriate for those with chronic low back pain and low back pain that is treatment resistant.
There is evidence that correction of leg length discrepancy with appropriate shoe lift therapy can successfully help those with chronic low back pain and/or back pain disabilities. Additionally, correction of pelvic obliquity and functional scoliosis early in life may prevent low back pain and disc disease/herniation; it may reduce the need for future spinal surgery and may improve surgical outcomes.
For individuals suffering from chronic low back pain, the combination of shoe lifts to compensate for leg length discrepancy, and chiropractic spinal adjusting (specific manipulations) to the spinal joints appears to be a biologically sound management approach.
REFERENCES
-
- Ramsey RH; Conservative Treatment of Intervertebral Disk Lesions; American Academy of Orthopedic Surgeons, Instructional Course Lectures; Volume 11; 1954; pp. 118-120.
- Mathews JA, Yates DAH; Reduction of Lumbar Disc Prolapse by Manipulation; British Medical Journal; September 20, 1969; No. 3; pp. 696-697.
- Edwards BC; Low back pain and pain resulting from lumbar spine conditions: a comparison of treatment results; Australian Journal of Physiotherapy; Vol. 15; 104; 1969.
- Turek S; Orthopaedics, Principles and Their Applications; JB Lippincott Company; 1977; page 1335.
- Kuo PP, Loh ZC; Treatment of Lumbar Intervertebral Disc Protrusions by Manipulation; Clinical Orthopedics and Related Research; No. 215; February 1987; pp. 47-55.
- Kirkaldy-Willis WH; Managing Low Back Pain; Churchill Livingston; (1983 & 1988).
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low-Back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-40.
- Quon JA, Cassidy JD, O’Connor SM, Kirkaldy-Willis WH; Lumbar intervertebral disc herniation: treatment by rotational manipulation; Journal of Manipulative and Physiological Therapeutics; June 1989; Vol. 12; No. 3; pp. 220-227.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine; Second edition; JB Lippincott Company; 1990.
- Meade TW, Dyer S, Browne W, Townsend J, Frank OA; Low back pain of mechanical origin: Randomized comparison of chiropractic and hospital outpatient treatment; British Medical Journal; Vol. 300; June 2, 1990; pp. 1431-7.
- Cassidy JD, Thiel HW, Kirkaldy-Willis WH; Side posture manipulation for lumbar intervertebral disk herniation; Journal of Manipulative and Physiological Therapeutics; February 1993; Vol. 16; No. 2; pp. 96-103.
- Stern PJ, Côté P, Cassidy JD; A series of consecutive cases of low back pain with radiating leg pain treated by chiropractors; Journal of Manipulative and Physiological Therapeutics; 1995 Jul-Aug; Vol. 18; No, 6; pp. 335-342.
- Giles LGF; Muller R; Chronic Spinal Pain: A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation; Spine July 15, 2003; Vol. 28; No. 14; pp. 1490-1502.
- Muller R, Giles LGF; Long-Term Follow-up of a Randomized Clinical Trial Assessing the Efficacy of Medication, Acupuncture, and Spinal Manipulation for Chronic Mechanical Spinal Pain Syndromes; Journal of Manipulative and Physiological Therapeutics; January 2005; Vol. 28; No. 1; pp. 3-11.
- Santilli V, Beghi E, Finucci S; Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion: A randomized double-blind clinical trial of active and simulated spinal manipulations; The Spine Journal; March-April 2006; Vol. 6; No. 2; pp. 131–137.
- Leemann S, Peterson CK, Schmid C, Anklin B, Humphreys BK; Outcomes of Acute and Chronic Patients with Magnetic Resonance Imaging–Confirmed Symptomatic Lumbar Disc Herniations Receiving High-Velocity, Low Amplitude, Spinal Manipulative Therapy: A Prospective Observational Cohort Study With One-Year Follow-Up; Journal of Manipulative and Physiological Therapeutics; March/April 2014; Vol. 37; No. 3; pp. 155-163.
- Adams J, Peng W, Cramer H, Sundberg T, Moore C; The Prevalence, Patterns, and Predictors of Chiropractic Use Among US Adults; Results From the 2012 National Health Interview Survey; Spine; December 1, 2017; Vol. 42; No. 23; pp. 1810–1816.
- Nachemson AL; The Lumbar Spine, An Orthopedic Challenge; Spine; Vol. 1; No. 1; March 1976, pp. 59-71.
- Mooney V; Where Is the Pain Coming From?; Spine; Vol. 12; No. 8; 1987; pp. 754-759.
- Kuslich S, Ulstrom C, Michael C; The Tissue Origin of Low Back Pain and Sciatica: A Report of Pain Response to Tissue Stimulation During Operations on the Lumbar Spine Using Local Anesthesia; Orthopedic Clinics of North America; Vol. 22; No. 2; April 1991; pp. 181-7.
- Izzo R, Popolizio T, D’Aprile P, Muto M; Spine Pain; European Journal of Radiology; May 2015; Vol. 84; pp. 746–756.
- Kapandji IA; The Physiology of the Joints; Volume 3; The Trunk and the Vertebral Column; Churchill Livingstone; 1974.
- Friberg O; Clinical Symptoms and Biomechanics of Lumbar Spine and Hip Joint in Leg Length Inequality; Spine; September 1983; Vol. 8; No. 6; pp. 643-651.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine; Second Edition; Lippincott; 1990.
- Cailliet R; Soft Tissue Pain and Disability; 3rd Edition; FA Davis Company; 1996.
- Oschman J; Energy Medicine, The Scientific Basis; Churchill Livingstone; 2000.
- Bowman K; Move Your DNA: Restore Your Health Through Natural Movement, Propriometrics Press; 2017.
- Rush WA, Steiner HA; A Study of Lower Extremity Length Inequality; American Journal of Roentgenology and Radium Therapy; Vol. 51; No. 5; November 1946; pp. 616-623.
- Bagg JE; The President’s Physician; Texas Heart Institute Journal; 2003; Vol. 30; No. 1; pp. 1–2.
- Wilson V; Janet G. Travell, MD: A Daughter’s Recollection; Texas Heart Institute Journal; 2003; Vol. 30; No. 1; pp. 8–12.
- Sicuranza B, Richards J, Tisdall L; The Short Leg Syndrome in Obstetrics and Gynecology; American Journal of Obstetrics and Gynecology; May 15, 1970; Vol. 107; No. 2; pp. 217-219.
- Giles LG, Taylor JR; Low-back pain associated with leg length inequality; Spine; 1981 Sep-Oct; Vol. 6; No. 5; pp. 510-251.
- Friberg O; Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality; Spine; 1983 Sep; Vol. 8; No. 6; pp. 643-651.
- Gofton JP; Persistent Low Back Pain and Leg Length Disparity; Journal of Rheumatology; Vol. 12, No. 4; August 1985; pp. 747-750.
- Helliwell M; Leg Length Inequality and Low Back Pain; The Practitioner; May 1985; Vol. 229; pp. 483-485.
- Defrin R, Benyamin SB, Dov Aldubi R, Pick CG; Conservative Correction of Leg-Length Discrepancies of 10 mm or Less for the Relief of Chronic Low Back Pain; Archives of Physical Medicine and Rehabilitation; November 2005; Vol. 86; No. 11; pp. 2075-2080.
- Golightly YM, Tate JJ, Burns CB, Gross MT; Changes in Pain and Disability Secondary to Shoe Lift Intervention in Subjects With Limb Length Inequality and Chronic Low Back Pain; Journal of Orthopaedic & Sports Physical Therapy; Vol. 37; No. 7; July 2007; pp. 380-388.
- Balik SM, Kanat A, Erkut A, Ozdemir B, Batcik OE; Inequality in Leg Length is Important for the Understanding of the Pathophysiology of Lumbar Disc Herniation; Journal of Craniovertebral Junction; Spine; April-June 2016; Vol. 7; No. 2; pp. 87-90.
- Cambron JA, Dexheimer JM, Duarte M, Freels S; Shoe Orthotics for the Treatment of Chronic Low Back Pain: A Randomized Controlled Trial; Archives of Physical Medicine and Rehabilitation; September, 2017; Vol. 98; No. 9; pp. 1752-1762.
- Sheha ED; Steinhaus ME; Kim HJ; Cunningham ME; Fragomen AT; Rozbruch SR; Leg-Length Discrepancy, Functional Scoliosis, and Low Back Pain; Journal of Bone and Joint Surgery Reviews; August 8, 2018; Vol. 6; No. 8; pp. e6.
- Travell J, Simons D; Myofascial Pain and Dysfunction, The Trigger Point Manual; New York: Williams & Wilkins, 1983.
- Keeney BJ, Fulton-Kehoe D, Turner JA, Wickizer TM, Chan KCG; Franklin GM; Early Predictors of Lumbar Spine Surgery after Occupational Back Injury: Results from a Prospective Study of Workers in Washington State; Spine; May 15, 2013; Vol. 38; No. 11; pp. 953-964.
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

