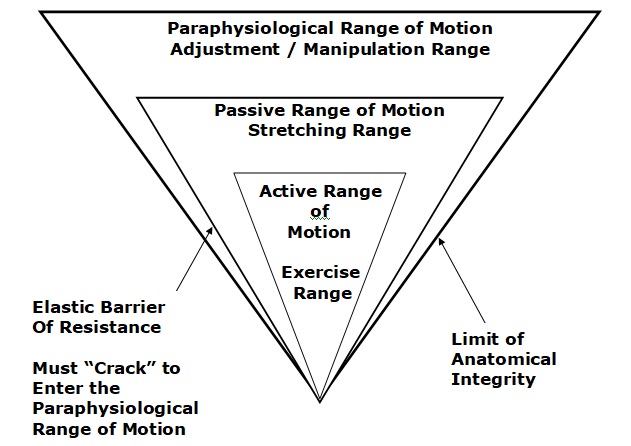
The chiropractic spinal adjustment (specific joint manipulation) is the passive assistance of moving a specific joint through a complete range of motion while causing no injury to the joint tissues. This adjustment is known for the cavitation process. Cavitation is the audible, palpable “popping” sensation experienced by both the patient and the chiropractor when the joint being adjusted is moved beyond the passive range of motion and into the paraphysiological range of motion. This motion is safe and causes no excessive stresses to tissues (1).
Spinal joints may lose their full ability to move through a range-of-motion for a number of reasons, including:
-
- Injury (whiplash, sports, lifting excessive loads, etc.)
- Chronic or prolonged mechanical stress (poor ergonomics and/or posture, excessive weight, etc.)
- Age related degenerative joint disease (arthritis)
This is important because when joints lose their full range-of-motion, they become painful. Motion activates nerves that suppress pain. This is a physiological principle that has been understood for decades (since 1965), and it is referred to as the “gate theory of pain.” Any therapeutic intervention that restores/improves the range of motion of joints suppresses the pain from that joint. Orthopedic Surgeon, Dr. WH Kirkaldy-Willis, MD, describes this phenomenon as (1):
“Beyond the end of the active range of motion of any synovial joint, there is a small buffer zone of passive mobility.” A joint can only move into this zone with passive assistance, and going into this passive range of motion “constitutes mobilization.”
“At the end of the passive range of motion, an elastic barrier of resistance is encountered. This barrier has a spring-like end-feel.”
“If the separation of the articular surfaces is forced beyond this elastic barrier, the joint surfaces suddenly move apart with a cracking noise.”
“This additional separation can only be achieved after cracking the joint and has been labeled the paraphysiological range of motion.” “This constitutes manipulation.”
“The cracking sound on entering the paraphysiological range of motion is the result of sudden liberation of synovial gases—a phenomenon known to physicists as cavitation.”
Melzack and Wall proposed the Gate Theory of Pain in 1965, and this theory has “withstood rigorous scientific scrutiny.”
“The central transmission of pain can be blocked by increased proprioceptive input.” Pain is facilitated by “lack of proprioceptive input.”
“Increased proprioceptive input in the form of spinal mobility tends to decrease the central transmission of pain from adjacent spinal structures by closing the gate. Any therapy which induces motion into articular structures will help inhibit pain transmission by this means.”
The joint cavitation that occurs during the chiropractic adjustment is a byproduct of joint motion.
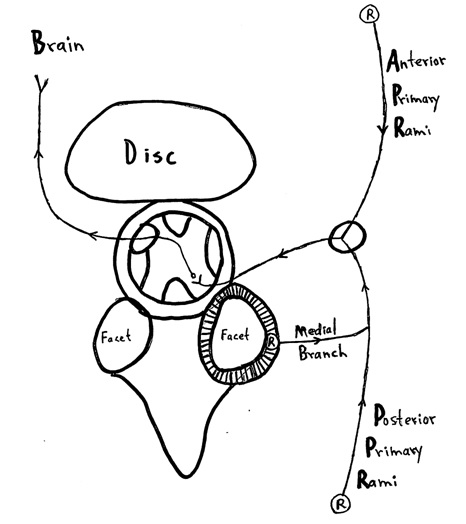
During the spinal adjustment, the primary joint to cavitate (“pop/crack”) is the facet (zygapophyseal) joint. Consequently, the adjustment and cavitation influence the facet joint capsular ligaments and the capsule’s neurology, as well as other effects on the joint’s muscles and cartilage.
Pain is an electrical signal that is sent to the brain. The pain electrical signal is carried into the brain by nerves. Therefore, the origin of the pain electrical signal must have a nerve supply. Every structure in the neck that has a nerve supply has the potential to cause pain.
In 1982 it was definitively established that the cervical spine facet joints are innervated with nociceptors, thus allowing the facet capsules to be a source of neck pain (2). By 1988, it became clear that the cervical spine facet joints were in fact a common source of neck pain (3). By 1992, it was established that the cervical spine facet joints were indeed the primary source of neck pain (4). This was confirmed in 2011 (5).
Cervical Spine Segmental Axial View
The facet joint capsule has nociceptors “R” which are connected to the brain through the medial branches of the posterior primary rami through the spinal cord.
The primary reason that people go to chiropractors is for the management of spine pain (6):
-
- 63% of chiropractic patients seek care for lower back pain
- 30% of chiropractic patients seek care for neck pain
Incredibly, 91% of these patients report acceptable positive clinical outcomes to chiropractic care for these complaints (6).
The percentage of individuals seeking chiropractic care for low back pain (63%) more than doubles the percentage of individuals seeking chiropractic care for neck pain (30%). Therefore, published studies and clinical practice guidelines have emphasized low back problems. Many of the recommendations for the management of patients with neck pain have been extrapolated from the low back pain literature, which may be inappropriate.
For low back pain, current recommendations from the Centers for Disease Control and Prevention (CDC) (7) and the American College of Physicians (ACP) (8, 9) for patients with low back pain favor non-pharmacological management as front-line treatment. It is clear that these non-drug management services are commonly offered by chiropractors.
The social and economic burdens of neck pain are immense, and neck pain is regarded as a major public health problem. Approximately half of all individuals will experience a clinically important neck pain episode over the course of their lifetime (10, 11).
The health care system entry point (ie, the type of provider a patient sees first) for an episode of low back pain affects downstream health care utilization and costs (12, 13, 14, 15). Presently, there is no consensus regarding the optimal provider to begin an episode of neck pain care, and hence it is unknown if first provider consulted for an episode of neck pain influences the long-term utilization of health care utilization and costs. Yet, a number of studies have compared the clinical outcome and service utilization between various providers for patients suffering with neck pain:
••••••••••
In 1996, a study was published in the journal Injury titled (16):
Chiropractic Treatment of Chronic ‘Whiplash’ Injuries
The 28 patients in this study had initially been treated with anti-inflammatory drugs, soft collars and physiotherapy. These patients had all become chronic, and were referred for chiropractic at an average of 15.5 months (range was 3–44 months) after their initial injury.
Following chiropractic 93% of the patients had improved. These authors state:
“The results of this retrospective study would suggest that benefits can occur in over 90% of patients undergoing chiropractic treatment for chronic whiplash injury.”
•••••••••••
In 2002, a study was published in the Annals of Internal Medicine, and titled (17):
Manual Therapy, Physical Therapy, or Continued Care by a
General Practitioner for Patients with Neck Pain:
A Randomized Controlled Trial
In this study, the authors compared the effectiveness of manual therapy, physical therapy, and care by a general practitioner (pharmacology) in the treatment of neck pain. They used a randomized controlled trial design. The study involved 183 patients. These authors concluded:
“Manual therapy scored consistently better than the other two interventions on most outcome measures.”
“In daily practice, manual therapy is a favorable treatment option for patients with neck pain compared with physical therapy or continued care by a general practitioner.”
“The success rates for manual therapy were statistically significantly higher than those for physical therapy.”
“Manual therapy scored better than physical therapy on all outcome measures…”
“Range of motion improved more markedly for those who received manual therapy or physical therapy than for those who received continued care.”
“The postulated objective of manual therapy is the restoration of normal joint motion, which was achieved, as indicated by the relatively large increase in the range of motion of the cervical spine.”
“Patients receiving manual therapy had fewer absences from work than patients receiving physical therapy or continued care.”
“Manual therapy seems to be a favorable treatment option for patients with neck pain.”
“Primary care physicians should consider manual therapy when treating patients with neck pain.”
••••••••••
In 2004, the American Academy of Orthopaedic Surgeons published a monograph titled Neck Pain (18). Chapter seven of the reference is titled “Manual Therapy Including Manipulation for Acute and Chronic Neck Pain.” This chapter is authored by a chiropractor and details the benefits of chiropractic spinal manipulation for the management of neck pain.
••••••••••
Also in 2004, the Journal of Whiplash & Related Disorders published a study titled (19):
Manipulative Treatment vs. Conventional Physiotherapy Treatment in Whiplash Injury: A Randomized Controlled Trial
This study assessed 380 acute whiplash injured patients. They found that manipulation therapy was superior to physical therapy (active exercises, electrotherapy, ultrasound therapy and diathermy). Specifically, spinal manipulation achieved a superior result in fewer patient visits as compared to the physical therapy group. The authors state:
“Patients who had received manipulative treatment needed fewer sessions to complete the treatment than patients who had received physiotherapy treatment.”
“Results showed that the manipulative group had more benefits than the physiotherapy group.”
“Our clinical experience with these patients [whiplash-injured] has demonstrated that manipulative treatment gives better results than conventional physiotherapy treatment.”
“This clinical trial has demonstrated that head and neck pain decrease with fewer treatment sessions in response to a manipulative treatment protocol as compared to a physiotherapy treatment protocol among patients diagnosed with acute whiplash injury.”
“Manipulative treatment is more effective in the management of whiplash injury than conventional physiotherapy treatment.”
••••••••••
A related and important study pertaining to neck pain and manipulation was published in 2015 in the Journal of Manipulative and Physiological Therapeutics and titled (20):
Prognostic Factors for Recurrences in Neck Pain Patients
Up to One Year After Chiropractic Care
This is a prospective cohort study assessing 545 neck pain patients. After a course of chiropractic, they were followed up for one year regarding recurrence of neck pain. The results of this study are impressive:
-
- Fifty-four (54) participants (11%) were identified as “recurrent.”
- Four hundred ninety-one (491) participants (89%) were not recurrent.
These authors concluded:
“The results of this study suggest that recurrence of neck pain within one year after chiropractic intervention is low.”
This study indicates that chiropractic is effective in the treatment of neck pain and that its benefits are stable and long lasting.
•••••••••
In 2017, a study was published in the journal Mayo Clinic Proceedings and titled (21):
Influence of Initial Provider on Health Care Utilization
in Patients Seeking Care for Neck Pain
The authors of this study were from the Department of Orthopaedic Surgery, Physical Therapy Division, Duke University, and from the Department of Physical Therapy, University of Utah. The authors note:
“It is imperative to evaluate the difference in health care process and outcomes in patients initially consulting with non-pharmacological providers (ie, chiropractors [DCs] and physical therapists [PTs]) and pharmacological providers (ie, specialists [such as physiatrists and neurologist]) in comparison to PCPs.”
This study looked at a cohort of patients seeking care for a new episode of neck pain to determine the association of the initial health care provider consulted and subsequent health care utilization. The health care utilization was assessed at 14 days, 30 days, and 1 year from the initial visit between various providers. The health care utilization assessed included:
-
- Imaging (MRI, computed tomography, radiography)
- Opioids
- Surgery (spinal arthrodesis, discectomy, laminectomy, or fusion)
- Injections (including nerve blocks)
The study used a retrospective cohort of 1,702 patients (69% women) with a new episode of neck pain who consulted a primary care provider (PCP), physical therapist (PT), chiropractor (DC), or specialist:
-
- PCP 44%
- DC 23%
- PT 17%
- Specialist (physiatrists, neurologist])16%
The authors also note:
“These specific provider types were included in the analysis because they are the most common providers consulted for neck pain.”
This is important, as it indicates that chiropractors are the second most consulted provider for neck pain.
The outcomes from this study are summarized as follows:
The Use of Interventions Compared to Primary Care Providers
(relative risk)
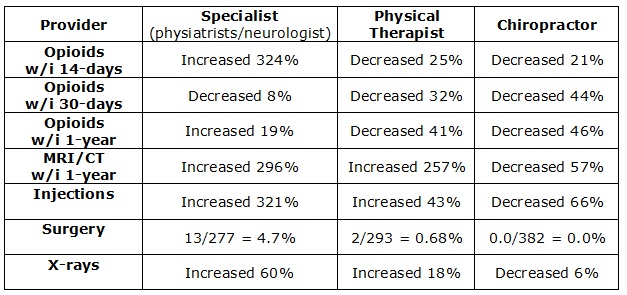
Based upon these results, the authors make the following important observations:
“Physical therapists and chiropractors primarily treat neck pain with exercise therapy and manual therapy, which has been found to have good effectiveness in treating nonspecific neck pain.”
In contrast, “primary care provider’s first line of treatment often includes medication, imaging, specialist referral, or a combination of those factors.”
“Initial consultation from either a chiropractor or physical therapist decreases the patient’s odds of being prescribed an opioid at 30 days or within any time in the 1-year follow-up period.”
Compared with initial consultation with a primary care provider, the odds of undergoing advanced imaging (MRI or computed tomography) within 1 year “was reduced when the initial provider was a chiropractor and increased when the initial provider was a specialist or a physical therapist.”
“When patients in the sample initially consulted with a chiropractor, the odds of MRI use decreased compared with consulting with a primary care provider.”
“We found that initial consultation with a non-pharmacological provider, such as a chiropractor or physical therapist, is associated with a decrease in the downstream utilization of health care services, and importantly a decrease in opioid use 30 days and 1 year after the initial consultation.”
“Initiating care with a specialist was associated with an increase in the odds of receiving spinal injections and undergoing MRI and radiography and had the highest percentage of patients undergoing surgery.”
“Initially consulting with a specialist for a new episode of neck pain appears to escalate the level of care patients with neck pain receive.”
“These findings support that initiating care with a non-pharmacological provider for a new episode of neck pain may present an opportunity to decrease opioid exposure (chiropractor and physical therapist) and advanced imaging and injections (chiropractor only).”
Pertaining to chiropractors and the use of spinal x-rays, these authors make these observations:
“Radiographic studies have been a longstanding mainstay of chiropractic practice.”
“Radiography is routinely ordered as part of a [chiropractic] treatment plan and is often performed at the initial visit.”
“It is plausible that the use of radiography may have paradoxically shielded patients from undergoing more advanced imaging such as MRI.”
“When a provider orders imaging, this can alleviate patients’ concern about serious pathology, despite a lack of evidence for clinical utility in routine care of patients with neck pain.”
The authors note that there are important practice and policy implications for the findings of this study. Current recommendations favor initial front-line use of non-pharmacological management for patients with neck pain. Yet, “many systems are not structured to provide care in this manner.” They state:
“Stronger alignment of physical therapists and chiropractors as front-line providers by health care systems may be needed in light of the widespread [drug] addiction, which has been identified as a public health epidemic.”
The public health epidemic of addiction to opioid drugs is particularly concerning, further emphasizing the need for non-drug approaches for neck pain. The authors commented that in addition to the decrease in odds of opioid prescription within 30 days of initial consultation of a non-drug provider, that this same decrease in odds persisted through the one-year follow-up assessment. This suggests that the clinical benefits from being managed by a non-drug provider resulted in a lasting protective influence in the treatment of neck pain.
THE IMPORTANCE OF CHIROPRACTIC
Compared to primary care physicians:
Chiropractors are the next most often consulted health care provider for the treatment of an acute episode of neck pain.
In every assessed parameter, chiropractic had the best outcomes, specifically:
-
- lowest rate of opioid prescription
- lowest use of advanced imaging
- lowest use of x-rays
- lowest referrals for injections
- lowest use (referrals) for surgery (in fact the number was zero).
These authors believe that practice guidelines should reflect their results and that healthcare systems and reimbursements should emphasize non-drug approaches to neck pain management.
These authors note that low back pain guidelines already advocate non-drug interventions as the primary approach and suggest that neck pain guidelines should “catch-up” with that perspective.
Ironically, these authors note that chiropractors are noted for the frequent use of spinal x-rays. They speculate that this increase in x-ray imaging may be responsible for the reduction of the use of advanced imaging, such as MRI and CT, resulting in a net benefit for both the patient and the reimbursing parties, saving the system monetary, time, and personnel resources.
REFERENCES:
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low Back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-540.
- Bogduk N; The clinical anatomy of the cervical dorsal rami; Spine; 1982 Jul-Aug; Vol. 7; No. 4; pp. 319-330.
- Bogduk N, Marsland A; The cervical zygapophysial joints as a source of neck pain; Spine; June 1988 Jun; Vol. 13; No. 6; pp. 610-617.
- Bogduk N, Aprill C; On the nature of neck pain, discography and cervical zygapophysial joint blocks; Pain; August 1993; Vol. 54; No. 2; pp. 213-217.
- Nikolai Bogduk; On Cervical Zygapophysial Joint Pain After Whiplash; Spine; December 1, 2011; Vol. 36; No. 25S; pp. S194–S199.
- Adams J, Peng W, Cramer H, Sundberg T, Moore C; The Prevalence, Patterns, and Predictors of Chiropractic Use Among US Adults; Results From the 2012 National Health Interview Survey; Spine; December 1, 2017; Vol. 42; No. 23; pp. 1810–1816.
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016; Journal of the American Medical Association; April 19 2016; Vol. 315; No. 15; pp. 1624-1645.
- Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians; Annals of Intern Medicine; 2017; Vol. 166; No. 7; pp. 514-530.
- Chou R, Deyo R, Friedly J, et al; Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline; Annals of Intern Medicine; 2017; Vol. 166; No. 7; pp. 493-505.
- Fejer R, Kyvik KO, Hartvigsen J; The prevalence of neck pain in the world population: a systematic critical review of the literature; European Spine Journal; 2006; Vol. 15; No. 6; pp. 834-848.
- Goode AP, Freburger J, Carey T; Prevalence, practice patterns, and evidence for chronic neck pain; Arthritis Care Res; 2010 Vol. 62; No. 11; pp. 1594-1601.
- Hurwitz EL, Li D, Guillen J, et al; Variations in patterns of utilization and charges for the care of neck pain in North Carolina, 2000 to 2009: a statewide claims’ data analysis; Journal of Manipulative and Physiological Therapeutics; 2016; Vol. 39; No. 4; pp. 240-251.
- Keeney BJ, Fulton-Kehoe D, Turner JA, Wickizer TM, Chan KCG, Franklin GM; Early Predictors of Lumbar Spine Surgery after Occupational Back Injury: Results from a Prospective Study of Workers in Washington State; Spine; May 15, 2013; Vol. 38; No. 11; pp. 953-964.
- Fritz JM, Kim J, Dorius J; Importance of the type of provider seen to begin health care for a new episode low back pain: associations with future utilization and costs; Journal of Eval Clinical Practice; 2016; Vol. 22; No. 2; pp. 247-252.
- Blanchette AM, Rivard M, Dionne CE, Hogg-Johnson S, Steenstra I; Association Between the Type of First Healthcare Provider and the Duration of Financial Compensation for Occupational Back Pain; Journal of Occupational Rehabilitation; September 2017; Vol 27; No. 3; pp. 382-392.
- Woodward MN, Cook JCH, Gargan MF, Bannister GC; Chiropractic treatment of chronic ‘whiplash’ injuries; Injury; November 1996; Vol. 27; No. 9; pp. 643-645.
- Hoving JC, Koes BW, de Vet HCW, van der Windt DAWM, Assendelft WJJ, Mameren H, Devillé WLJM; Manual Therapy, Physical Therapy, or Continued Care by a General Practitioner for Patients with Neck Pain; A Randomized Controlled Trial; Annals of Internal Medicine; May 21, 2002; Vol. 136; No. 10; pp. 713-722.
- Fischgrund JS; Neck Pain, Monograph 27, American Academy of Orthopaedic Surgeons; 2004.
- César Fernández-de-las-Peñas; J. Fernández-Carnero; L. Palomeque del Cerro; Manipulative Treatment vs. Conventional Physiotherapy Treatment in Whiplash Injury: A Randomized Controlled Trial; Journal of Whiplash & Related Disorders; 2004; Vol. 3; No. 2.
- Langenfeld A, Humphreys K, Swanenburg J, Cynthia K. Peterson CK; Prognostic Factors for Recurrences in Neck Pain Patients Up to 1 Year After Chiropractic Care; Journal of Manipulative and Physiological Therapeutics; September 2015; Vol. 38; No. 7; pp. 458-464.
- Horn ME, George SZ, Fritz JM; Influence of Initial Provider on Health Care Utilization in Patients Seeking Care for Neck Pain; Mayo Clinic Proceedings: Innovations, Quality & Outcomes; October 19, 2017; Vol. 1; No. 3; pp. 226-233.
Atlas Health Solution
Our Goal
To provide safe and effective, fast and reliable PAIN RELIEF without the use of pharmaceutical drugs.

