The total sum of suffering caused by migraine is higher than any other kind of headache (1). “Migraine is often incapacitating, with considerable impact on social activities and work, and may lead to significant consumption of drugs.” (1)
The diagnosis of migraine is made clinically. There are no blood tests, imaging, or electro-physiologic tests to establish the diagnosis (1).
The strict definition of migraine headache is (2):
-
- The headache must last 4 to 72 hours.
- The headache must be associated with nausea and/or vomiting, or photophobia, and/or phonophobia.
- The headache must be characterized by 2 of the following 4 symptoms: unilateral location; throbbing pulsatile quality; moderate or worse degree of severity; intensified by routine physical activity
The migraine diagnosis is assured when these characteristics are present:
-
- The headache is episodic
- The pain involves half the head
- There is an aura
- There are associated gastrointestinal symptoms
- There is photophobia and/or phonophobia
- The pain is aggravated by the Valsalva maneuver and/or by the head-low position
- The migraine attacks are triggered by: The menstrual cycle; Fasting; Oversleeping; Indulgence in alcohol; Tyramine-containing foods [meats that are pickled, aged, smoked, fermented; most pork; chocolate; and fermented foods, such as most cheeses, sour cream, yogurt, soy sauce, soybean condiments, teriyaki sauce, tempeh, miso soup, and sauerkraut]
- Migraine relief occurs with sleep
••••••••••
An article appearing in the Business Section of the San Francisco Chronicle newspaper on July 20, 2014, stated (3):
MEDICINE
Huge Headache of a Problem
Mastering Migraines Still a Challenge for Patients, Scientists
The author, Stephanie Lee, notes that 36 million Americans suffer from migraine headaches. The migraine market in developed countries will grow to about $5.4 billion in 2022. The problem is that current treatments are not very effective and they may have dangerous side effects. Ms. Lee notes (3):
“Frustrated patients often seek out opioids in the emergency room, but opioids can be dangerous. In a year, … 20,000 patients in California developed chronic migraines because of opioid overuse, and 3,000 become addicted.”
Chronic migraine is defined as a severe headache that occurs at least 15 times per month. It is ironic that opioids taken for migraines cause chronic migraines in many patients. Ms. Lee concludes (3):
“The demand for safe and effective alternatives [for migraine headaches] is urgent.”
Evidence is mounting that chiropractic and spinal manipulation may provide this sought-after safe and effective alternative.
••••••••••
In the modern era of musculoskeletal clinical anatomy, Australia’s Nikoli Bogduk, MD, PhD, is perhaps the most accomplished and respected. A search of the National Library of Medicine using the PubMed search engine with “bogduk n”, locates 259 references (as of May 12, 2017). In addition, Dr. Bogduk has written numerous books, chapters in books, and invited opinion/editorials. His expertise in clinical anatomy has extended for four decades, and continues through today.
Dr. Bogduk’s expertise in clinical anatomy includes the field of headache. A PubMed search using the words “Bogduk N and Headache” finds 25 citations (as of May 12, 2017). Perhaps his most important contribution to the understanding of the clinical anatomy of headache appeared in the journal Biomedicine and Pharmacotherapy in 1995. The article is titled (4):
Anatomy and Physiology of Headache
In this article, Dr. Bogduk details the clinical anatomy of headaches, noting that “all headaches have a common anatomy and physiology,” including migraine headache. Specifically, he states:
“All headaches are mediated by the trigeminocervical nucleus.”
Specifically, this means that all headaches, including migraine headaches, synapse in the upper aspect of the neck, in a location termed the trigeminocervical nucleus. The brainstem and the upper cervical spinal cord contain a contiguous region of grey matter, the trigeminocervical nucleus.
The trigeminocervical nucleus is “defined by its afferent fibers.” The primary afferent fibers to the nucleus are from the Trigeminal Nerve (Cranial Nerve V), and from the upper three cervical nerves (C1, C2, C3), and hence the name trigeminocervical nucleus. All headaches synapse in the trigeminocervical nucleus. Second order afferent neurons arising in the trigeminocervical nucleus ascend to create an electrical signal in the brain that is interpreted as “headache.”
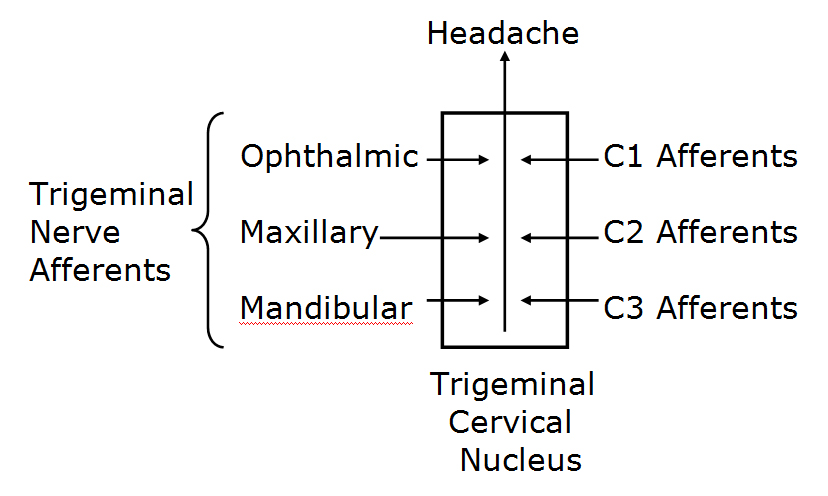
Consequently, upper cervical spine afferents to a second-order neuron that also receives trigeminal input may be a source of the electrical signal that is interpreted as headache in the brain, including migraine headache. As such, structures that are innervated by C1, C2, C3, can cause headache, including migraine. Irritation and/or inflammation of structures innervated by C1, C2, C3 can all cause headaches. Such structures include:
-
- Dura mater of the posterior cranial fossa
- Inferior surface of the tentorium cerebelli
- Anterior and posterior upper cervical and cervical-occiput muscles
- OCCIPUT-C1, C1-C2, and C2-C3 joints
- C2-C3 intervertebral disc
- Vertebral arteries
- Carotid arteries
- Alar ligaments
- Transverse ligaments
- Trapezius muscle
- Sternocleidomastoid muscle
••••••••••
Recent Clinical Studies
In June 2014, Dean Watson and Peter Drummond from Murdoch University, Perth, WA, Australia, published a study in the journal Headache, titled (5):
Cervical Referral of Head Pain in Migraineurs:
Effects on the Nociceptive Blink Reflex
This study assessed the pain intensity and nociceptive blink reflex in 15 migraine subjects between times of symptoms with passive movements of the occipital and upper cervical spinal segments. The nociceptive blink reflex was elicited with a supraorbital electrical stimulus. The number of blinks of the nociceptive blink reflex were recorded. Head pain intensity was graded from 0-10, where 0 = “no pain” and 10 = “intolerable pain.” They note:
-
- Anatomical and neurophysiological studies show that there is a functional convergence of trigeminal and cervical afferent pathways.
- Migraine patients often have occipital and neck symptoms, with cervical pain being referred to the head, “suggesting that cervical afferent information may contribute to [migraine] headache.”
- Nerve blocks of the greater occipital nerve [C-2] modulate migraine pain, demonstrating a role for cervical afferents in migraine.
- “Spinal mobilization is typically applied when dysfunctional areas of the vertebral column are found.” “The clinician’s objective in applying manual techniques is to restore normal motion and normalize afferent input from the neuromusculoskeletal system.”
- There is a functional influence on trigeminal nociceptive inputs from cervical afferents. This study showed that passive manual intervertebral movement between the occiput and the upper cervical spinal joints decreases excitability of the trigeminocervical nucleus.
- “Our findings corroborate previous results related to anatomical and functional convergence of trigeminal and cervical afferent pathways in animals and humans, and suggest that manual cervical modulation of this pathway is of potential benefit in migraine.” [emphasis added]
- These findings show that “cervical spinal input contributed to lessening of referred head pain and cervical tenderness.”
These authors conclude:
Ongoing noxious sensory input arises from biomechanically dysfunctional spinal joints. Mechanoreceptors including proprioceptors (muscle spindles) within deep paraspinal tissues react to mechanical deformation of these tissues. Manual mechanical deformation can cause “biomechanical remodeling” with restoration of zygapophyseal joint mobility and joint “play.” “Biomechanical remodeling resulting from mobilization may have physiological ramifications, ultimately reducing nociceptive input from receptive nerve endings in innervated paraspinal tissues.”
These findings “corroborate previous results related to anatomical and functional convergence of trigeminal and cervical afferent pathways in animals and humans, and suggest that manual modulation of the cervical pathway is of potential benefit in migraine.”
This article supports the clinical anatomical perspective of Dr. Bogduk. It also extends the concept for the inclusion of manual/manipulative therapy of the cervical spine in the management of chronic migraine headache.
••••••••••
The following year, 2015, the journal Complementary Therapies in Medicine, published a study titled (6):
Clinical Effectiveness of Osteopathic Treatment in Chronic Migraine:
3-Armed Randomized Controlled Trial
The primary measurement outcome in this study was the Headache Impact Test-6. The Headache Impact Test-6 was validated in the journal Cephalalgia in 2011, with the following conclusions (7):
“Our study shows that the Headache Impact Test-6 is a reliable and valid tool for measuring the impact of headache on daily life in both episodic and chronic migraine sufferers. Furthermore, the Headache Impact Test-6 tool discriminates well between chronic migraine, episodic migraine and non-migraine patients.”
“As a brief tool, the Headache Impact Test-6 is easy to score and interpret, and can be readily integrated into clinical practice, or clinical studies of migraine patients. It may offer clinicians a practical and easy-to-implement tool to assist them with evaluating treatment effectiveness by obtaining input directly from the patient on aspects other than just the frequency of headache days.”
The authors of this study note that this manipulative therapy trial is the largest ever conducted on adult migraine patients. The authors assessed the effectiveness of manipulative treatment on 105 chronic migraine patients using:
-
- Headache Impact Test (HIT-6) questionnaire (main outcome measure)
- Drug consumption
- Days of migraine
- Pain intensity
- Functional disability
This is a randomized controlled trial. Patients received 8 treatments over a period of 6 months. Patients were randomly divided into three groups:
- Manipulation + medication therapy (n=35) – The manipulative techniques used in this study included myofascial release, treatment of ligamentous and membrane tensions, treatment of somatic dysfunctions, and treatment to asymmetries and imbalances in the pelvis and cranium.
- Sham manipulation + medication therapy (n=35) – The sham group received a false manipulation, in addition to drug care. Sham therapy mimicked the manipulative care in terms of evaluation and treatment; it used light manual contact to ‘‘treat’’ the subject. Both manipulative and sham therapy sessions lasted 30 minutes and were given weekly for the first two sessions, biweekly for the subsequent two, then monthly for the remained four sessions.
- Medication only (n=35)
The criteria considered for manipulative evaluation and treatment were:
-
- Alteration of tissue consistency
- Asymmetry
- Range of motion restriction
- Tenderness
The authors note that manipulation in migraine could reduce the release of pro-inflammatory substances that have an effect on the nociceptive nervous system. They state:
“As a consequence [of manipulation], a cascade of biological and neurological events, potentially based on a rebalance of the abnormal activation of the habituation/sensitization mechanism, even between attacks, could occur resulting in an overall improvement of clinical outcomes.”
Key findings from this study include:
-
- At the end of the study period, there was a statistically significant difference on the overall HIT-6 score between the three groups; the manipulation group was statistically improved from control (drug only) and sham group.
- Manipulation “significantly reduced the frequency of migraine.”
- Manipulation “significantly reduced the number of subjects taking medications.”
- “No study participant reported any adverse effects of the [manipulation].”
- Manipulation “showed a significant improvement in the migraineurs’ quality of life.”
- The use of manipulative therapy as an “adjuvant therapy for migraine patients may reduce the use of drugs and optimize the clinical management of the patients.”
- Manipulation “may be considered a clinically valid procedure for the management of patients with migraine.”
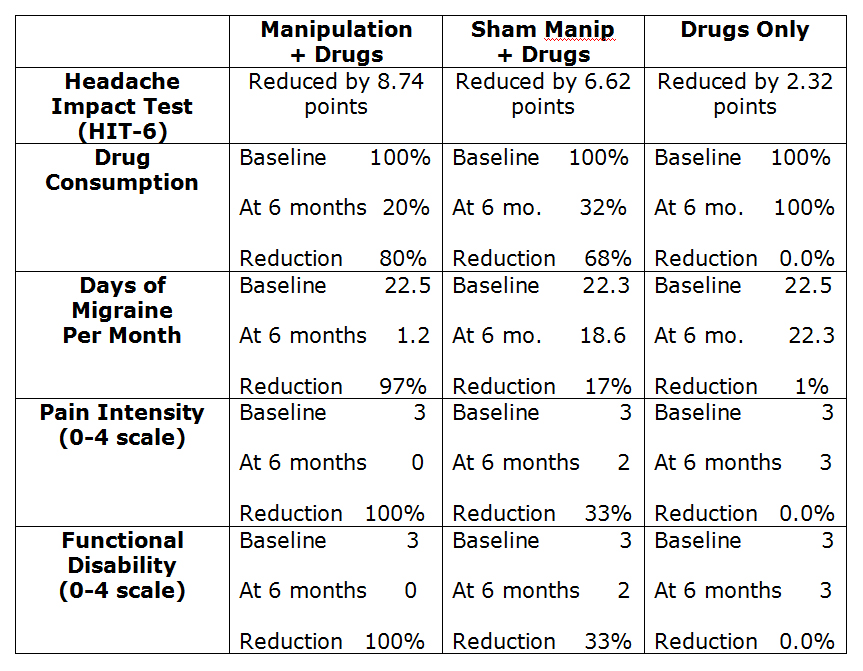
The following remarkable graph was presented in the study:
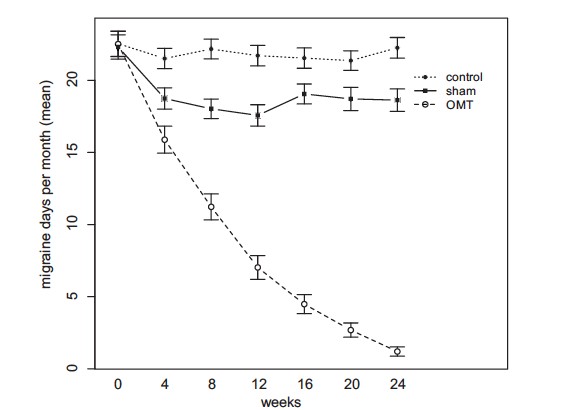
The data indicates that the manipulation essentially eliminated migraine days per month, including pain and disability, and reduced drug consumption by 80%. For the group assigned to taking drugs-only, there was essentially no reduction in migraine days per month, pain, disability, and no reduction in drug consumption.
••••••••••
In 2017, researchers from Akershus University Hospital, Oslo, Norway, and the Department of Chiropractic, Macquarie University, NSW, Australia, published a study in the journal Musculoskeletal Science and Practice titled (8):
Adverse Events in a Chiropractic Spinal Manipulative Therapy:
Single-blinded, Placebo, Randomized Controlled Trial for Migraineurs
The primary objective of this study was to “report on all adverse events in a prospective chiropractic spinal manipulative therapy, single-blinded, placebo, randomized controlled trial for migraineurs.”
The authors note that migraines are a common worldwide challenge, and pharmacological management is often the first treatment of choice. However, migraine drugs can have serious and/or undesirable side effects. In contrast, manual-therapy is a non-pharmacological migraine treatment option that appears to have a similar effect as common drugs on migraine frequency, migraine duration, and migraine intensity.
This study prospectively reported all adverse events in a chiropractic spinal manipulative therapy randomized controlled trial. It is a prospective assessment; 70 migrainers were randomized to chiropractic manipulation (Gonstead full-spine adjusting) or a placebo, with 12 intervention sessions over three months. The subjects in this study were randomly placed into three groups:
- An active spinal manipulation group, using Gonstead technique: “Active treatment consisted of chiropractic spinal manipulation using the Gonstead method, i.e., a specific contact, high-velocity, low-amplitude, short-lever spinal with no post-adjustment recoil that was directed to spinal biomechanical dysfunction (full spinal column approach) as diagnosed by standard chiropractic tests performed during each individual treatment session.”
- A placebo manipulation group, receiving sham manipulation: “The placebo intervention consisted of sham manipulation, i.e., a broad non-specific contact approach via a low-velocity, low-amplitude sham push manoeuvre in a non-intentional and nontherapeutic directional line. All of the non-therapeutic contacts were performed outside the spinal column and included adequate joint ligament slack without soft tissue pre-tension so that joint cavitations did not occur.”
- A control group, using usual pharmacological management: “The control group continued their usual pharmacological management without receiving manual intervention.”
The participants were interviewed and physically assessed by a chiropractor, “including meticulous investigation of the spinal column.” They also received a full spine radiographic examination. The subjects attended 12 intervention sessions over 12 weeks with follow-up at 3, 6 and 12 months post-treatment. The authors concluded:
This study “showed significant differences between the chiropractic spinal manipulation group and the control group [drug group] at all post-treatment time points.”
“Local tenderness, tiredness and neck pain were the most common adverse events, whereas other adverse events were rare (<1%).”
“Conclusions: Adverse events [to spinal manipulation] were mild and transient, and severe or serious adverse events were not observed.”
“These findings are in accordance with the World Health Organization guidelines on basic training and safety in chiropractic spinal manipulation, which is considered to be an efficient and safe treatment modality (WHO, 2005).” (9)
“Adverse events in migraine prophylactic pharmacological randomized clinical trials are common. The risk for adverse events during manual-therapy [is] substantially lower than the risk accepted in any medical context for both acute and prophylactic migraine medication.”
Non-pharmacological management of migraine has the advantage of having mild and transient adverse events, “whereas pharmacological adverse events tend to be continuous.”
“Chiropractic spinal manipulation applying the Gonstead technique appears to be safe for the management of migraine headache and presents few mild and transient adverse events.”
This study used Gonstead analysis, full-spine x-rays, and full-spine adjusting, for patients with chronic migraines. Although this Gonstead adjusting resulted in a few adverse events, they were minor and transient. Additionally, the chiropractic adjusting had the best long-term results.
••••••••••
Summary
These studies explain what essentially every chiropractor has observed:
Improvement of the mechanical function of the upper cervical spine with spinal manipulation and other adjunctive mechanical interventions is effective and safe intervention for patients suffering from chronic migraine headache.
The presented data here suggests that manipulation actually addresses the causative pathophysiology of migraine headache; in contrast, it appears that taking drugs is nothing more than temporary pain control with no improvement to the causative pathophysiology of migraine headache.
REFERENCES
- Olsen J, Tfelt-Hansen P, Welch KMA; The Headaches, second edition; Lippincott Williams & Wilkins; 2000.
- Jones HR, MD; Netter’s Neurology; 2005.
- Lee, SM; Huge Headache of a Problem; Mastering Migraines Still a Challenge for Patients, Scientists; San Francisco Chronicle; July 20, 2014; pp. D1 and D5.
- Bogduk N; Anatomy and Physiology of Headache; Biomedicine and Pharmacotherapy; 1995, Vol. 49, No. 10, 435-445.
- Watson DH, Drummond PD; Cervical Referral of Head Pain in Migraineurs: Effects on the Nociceptive Blink Reflex; Headache 2014; Vol. 54; pp. 1035-1045.
- Cerritelli F, Ginevri L, Messi G, Caprari E, Di Vincenzo M, Renzetti C, Cozzolino V, Barlafante G, Foschi N, Provincial L; Clinical Effectiveness of Osteopathic Treatment in Chronic Migraine: 3-Armed Randomized Controlled Trial; Complementary Therapies in Medicine; April 2015; Vol. 23; No. 2; pp. 149—156.
- Yang M, Rendas-Baum R, Varon SF, Kosinski M; Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine; Cephalalgia; 2011 Feb; 31(3): 357–367.
- Chaibi A, Benth JS, Tuchin PJ, Russell MB; Adverse Events in a Chiropractic Spinal Manipulative Therapy Single-blinded, Placebo, Randomized Controlled Trial for Migraineurs; Musculoskeletal Science and Practice ; March 2017; Vol. 29; pp. 66-71.
- WHO, 2005. Guidelines on Basic Training and Safety in Chiropractic. World Health Organization, Switzerland.
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

