Pain is a big problem in America. Of the 238 million adults in America, approximately 116 million suffer from chronic pain (1, 2, 3). The majority of pain and its suffering are musculoskeletal, and is quantified by body region as follows (4):
Lower-Back Pain 28.1%
Knee Pain 19.5%
Severe Headache 16.1%
Neck Pain 15.1%
Shoulder Pain 09.0%
Finger Pain 07.6%
Hip Pain 07.1%
As noted, the most common location for chronic pain is the low back. Back pain and neck pain combined account for approximately 43% of chronic pain.
It is no longer controversial to understand that chiropractic and spinal manipulation are safe and effective treatments for neck and back pain (5, 6, 7, 8, 9, 10, 11, 12, 13). It is also commonplace for spine pain clinical practice guidelines to include chiropractic and/or spinal manipulation (14, 15, 16).
Treating chronic spinal pain has always been a challenge for health care providers. An advance in the battle was achieved in 1973. Candace Beebe Pert (June 26, 1946 – September 12, 2013) was an American neuroscientist and pharmacologist who discovered the opiate receptor, the cellular binding site for endorphins in the brain (17). In 1974 Candace Pert earned a Ph.D. in pharmacology from Johns Hopkins University School of Medicine, where she worked in the laboratory of Solomon Snyder and discovered the brain’s opiate receptor. Pert’s and Snyder’s discovery of the opiate receptor drastically changed the approach to the management of chronic pain sufferers.
By 1977, researchers determined that the opiate receptors in the upper brain stem (mesencephalon) were responsible for controlling pain throughout the body (18). The specific location for these opiate receptors was the grey matter surrounding the cerebral aqueduct, known as periaqueductal gray matter:
Mesencephalon
Periaqueductal Gray Matter
Axial View
posterior
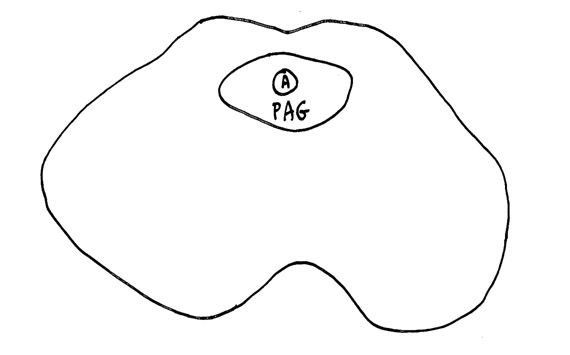
anterior
The authors from the 1977 article inserted electrodes into the periaqueductal gray matter of the mesencephalon of six cancer patients suffering from intractable pain. They state (18):
“Relief of intractable pain was produced in six human patients by stimulation of electrodes permanently implanted in the periventricular and periaqueductal gray matter.”
In his 1979 book, The Brain, The Last Frontier, Richard Restak, MD, reviews this research, stating (19):
“Within the periaqueductal gray, a deep-seated brainstem area lying along the floor of the third ventricle, neurosurgeons at the University of California in San Francisco placed indwelling stimulating electrodes for pain relief in six patients afflicted with chronic, unremitting pain. Whenever the patients began to experience pain, they were able to shut it off via the activation of a battery-operated stimulator about the size of a pack of cigarettes. After activating the stimulator, all six patients—in accordance with earlier findings in other pain patients—experienced dramatic, long-lasting, and repeatable pain relief.”
“In order to test the hypothesis that pain relief was genuine and not just an example of a ‘placebo response,’ one patient was outfitted with a stimulator containing a ‘dead’ battery. The patient, a fifty-one-year-old woman with severe back and leg pain caused by cancer of the colon, anxiously reported that her pain had returned and the stimulator ‘wasn’t working.’ Replacement of a new battery led to immediate pain relief.”
Periaqueductal gray matter stimulation for pain control initiates what is today know as activating the Descending Pain Inhibitory Control System, and it has continued to receive reference text support decades later:
-
- Barr’s The Human Nervous System, An Anatomical Viewpoint, John A Kiernan, Lippincott-Raven, 1998, pp351-352.
Descending pathways modify the activity of all ascending systems, including responses to noxious stimuli.
The best understood of these is the raphespinal tract, which arises from neurons in the raphe nuclei of the medullary reticular formation, mainly those of the nucleus raphes magnus, and use serotonin as a neurotransmitter.
The nucleus raphes magnus is itself influenced by descending fibers from the periaqueductal gray matter of the midbrain.
Electrical stimulation of the nucleus raphes magnus or the periaqueductal gray matter causes profound analgesia.
An electrode sterotaxically implanted into the periaqueductal gray matter enables a patient to relieve pain instantly when switching on an electrical stimulator. The analgesia often lasts for several hours after cessation of the stimulation.
-
- The Human Brain, An Introduction To Its Functional Anatomy, John Nolte, Mosby, 1999, pp. 270-271, p. 274.
Electrical stimulation (through implanted electrodes) of the periaqueductal gray of the midbrain causes analgesia so profound that major surgery can then be performed without the aid of an anesthetic.
Stimulation of the periaqueductal gray of humans can ameliorate intractable pain.
The periaqueductal gray receives inputs from the hypothalamus and several cortical areas.
Opium and its derivatives, especially morphine, have long been used for pain control, and one way they work is by activating the periaqueductal gray-raphe nucleus pain-control system at multiple levels.
Opiate receptors are found in abundance in the periaqueductal gray, nucleus raphe magnus, and superficial laminae of the posterior horn.
Opiate receptors are also found at a number of other sites in the CNS, accounting for some of the other effects of morphine and related drugs.
-
- Principles of Neural Science, Eric Kandel, et.al., 2000, pp. 482-485.
Stimulation of the periaqueductal gray region produces a profound analgesia.
Periaqueductal gray neurons make excitatory connections with neurons of the rostroventral medulla, in particular with serotonergic neurons in the midline of the nucleus raphe magnus.
Opiates such as morphine and codeine are effective analgesic agents.
The periaqueductal gray region is the most sensitive site for eliciting opiate (such as morphine) induced analgesia.
Morphine and other opiates produce analgesia by activating descending inhibitory pathways. Morphine is a chemical that binds to opioid peptide receptor sites and causes powerful analgesia.
Opiate receptors are found in many other sites of the central and peripheral nervous systems, which explains the many other physiological effects of systemically administered morphine.
-
- Functional Neuroscience, Oswald Steward, Springer, 2000, pp. 218-219.
An important aspect of nociception is that transmission along pain pathways is modulated by descending systems.
Stimulation of the periaqueductal gray matter leads to a loss of sensitivity to painful stimuli.
This finding led to the development of therapies for intractable pain that involved stimulating the periaqueductal gray with implanted electrodes. Such stimulation alleviates pain.
Descending modulation of pain sensitivity is mediated by the descending projections from the periaqueductal gray.
The descending circuits that modulate transmission along nociceptive pathways are thought to operate in part by using opioid peptides as their neurotransmitter.
Opiate-containing neurons in the periaqueductal gray and medulla activate neurons that give rise to the descending pathways.
Together, these studies indicate the following:
-
- Opiate receptors, when activated, inhibit pain.
- The periaqueductal gray matter of the mesencephalon is densely populated with opiate receptors.
- Electrical stimulation of the periaqueductal gray matter opiate receptors causes quick and complete pain relief throughout the body.
As such, one might ask, why are not all chronic pain patients treated with electrical stimulation to the periaqueductal gray matter of the mesencephalon? Although effective, there are serious logistical problems with such an approach to pain control. Inserting an electrode into the periaqueductal gray matter necessitates breaching the integrity of the blood brain barrier. The blood brain barrier integrity is of upmost importance in protecting the integrity of the brain and spinal cord (20):
The blood brain barrier confers “precise control of central nervous system homeostasis allows for proper neuronal function and also protects the neural tissue from toxins and pathogens, and alterations of these barrier properties are an important component of pathology and progression of different neurological diseases.”
As a consequence of this logistical hurdle, the primary contemporary clinical approach to chronic pain treatment by activating the periaqueductal gray matter descending pain inhibitory control system is pharmacology, and over the past decade that has been an over-emphasization in the use of opioid pharmacology. This has created a modern day nightmare because:
-
- As noted above, opiate receptors are found throughout the nervous system. Besides suppressing pain, opiate pharmacology is notorious for causing euphoria and serious, life threatening, addictions.
- Chemical activation of the opiate receptors causes rapid receptor adaptation. This means that after a short time of using these pharmacological products, their benefit diminishes. Provider choices are to increase the dose or add a second opiate drug. Sadly, this approach broadens the receptor adaptation issue, and a dangerous scenario may follow:
- The June 15, 2015 cover article of the political magazine Time states (21):
“They’re the most powerful painkillers ever invented. And they’re creating the worst addiction crisis America has ever seen.”
“…9.4 million Americans take opioids for long-term pain.”
“Doctors so frequently prescribe the drugs known as opioids for chronic pain from conditions like arthritis, migraines and lower back injuries that there are enough pills prescribed every year to keep every American adult medicated around the clock for a month.”
“Now 4 of 5 [80%] heroin addicts say they came to the drug from prescription painkillers.”
“The American Academy of Neurology last year concluded that the risks of long-term opioid treatment for headaches and chronic low-back pain likely outweigh the benefits.”
-
- The November/December issue of the RandReview published an article titled Opioid Rising, which notes (22):
Heroin kills more than 8,000 Americans yearly, but opioid prescription painkillers kill more double that number.
“The Centers for Disease Control and Prevention now considers opioid drug abuse to be a full-fledged epidemic.”
-
- Recent publications indicate that 78 Americans die daily from opioid painkillers overdoses (23).
Potential Solutions
The spine is a very complex system. As a profession, chiropractic has many specializations, including some who specialize in biomechanical problems of the neck, and others that specialize in biomechanical problems of the low back. An interesting anecdote is the clinical observation of spinal manipulation in one region of the body alleviating pain in a different, untreated region of the body; this can pertain to other spinal regions, extremities, head, etc. It is for this reason that many chiropractors adjust (specific manipulation) only proven biomechanical lesions, regardless of the patient’s pain presentation.
This approach to treating the spine (treat the biomechanical problem v. the place of pain) is not new. Reference texts have for decades noted that the spine is a single functioning unit; this means that necks and back are functionally integrated, and vise versa:
-
- The editors of The Spine, Richard Rothman, MD, PhD, and Frederick Simeone, MD, published the second edition of their book in 1982 (24). Their book also includes 30 distinguished contributing authors. Chapter 2 of the book is titled (25):
“Applied Anatomy of the Spine”
This chapter is written by Wesley Parke, PhD. In 1982, Dr. Parke was Professor and Chairman, Department of Anatomy, University of South Dakota School of Medicine. In this chapter, Dr. Parke writes:
“Although the 23 or 24 individual motor segments must be considered in relation to the spinal column as a whole, no congenital or acquired disorder of a single major component of a unit can exist without affecting first the functions of the other components of the same unit and then the functions of other levels of the spine.”
I believe that the point of Dr. Parke’s comments is that although spinal biomechanical function and pathology is often discussed in terms of the segmental motor unit and all of its components, that in fact the entire spinal column is an integrated functioning unit. Specifically, this would indicate that a cervical spine disorder could influence the function and symptomatology of the lower back, and visa versa.
The concept of the entire spine acting as a single integrated functioning entity is further supported by the reference text written by rheumatologist John Bland, MD, in his 1987 text:
Disorders of the Cervical Spine
Dr. Bland is a Professor of Medicine at the University of Vermont College of Medicine. Dr. Bland writes:
“We tend to divide the examination of the spine into regions: cervical, thoracic, and lumbar spine clinical studies.
This is a mistake.
The three units are closely interrelated structurally and functionally – a whole person with a whole spine.
The cervical spine may be symptomatic because of a thoracic or lumbar spine abnormality, and vice versa!
Sometimes treating a lumbar spine will relieve a cervical spine syndrome, or proper management of cervical spine will relieve low backache.”
In addition to these biomechanical considerations, published studies are showing a neurological explanation for the reason that spinal adjusting is capable of relieving pain in body regions that are not treated. Interestingly, these explanations involve the activation of the periaqueductal gray matter descending pain inhibitory control system.
In 1996, Bill Vicenzino, David Collins, and Anthony Wright from the University of Queensland published a study in the journal Pain, titled (27):
The Initial Effects of a Cervical Spine Manipulative Physiotherapy Treatment on the Pain and Dysfunction of Lateral Epicondylalgia
Importantly, these authors were treating elbow pain in patients who are not suffering from radiculopathy or referred pain without touching or treating the offending elbow. In contrast, treatment was directed towards the dysfunctional joints of the patient’s cervical spine. The most commonly found biomechanical dysfunction was hypomobility of the joints of the lower cervical spine. The authors made the following comments:
“This study has demonstrated a clear hypoalgesic effect of a manipulative therapy technique [applied to the cervical spine] in the period immediately following its application in a group of patients with lateral epicondylalgia.”
“A significant treatment effect beyond placebo or control was demonstrated.”
“The beneficial effects of treatment [cervical manipulation] may continue after its application.”
The author’s theoretical model to explain their results involved manipulative therapy activation of the hypoalgesic effects of the endogenous supraspinal pain inhibitory systems.
“The [manipulative] treatment technique used in this study provided a non-noxious sensory input at the cervical spine which resulted in a reduction of elbow pain that outlasted the duration of its application.” “This is thought to activate the descending pain inhibitory system as a major component of their pain-relieving effects.”
The descending pain inhibitory system is activated by stimulation of the periaqueductal gray (PAG).
“These findings indicate that manipulative therapy may constitute an adequate physical stimulus for activating descending pain inhibitory system.”
A common finding in other studies “was the predominance of hypomobility at the lower cervical motion segments.” It is feasible that part or all of the impairments in this study were “projected from the hypomobile cervical spine motion segment(s), and that the improvements gained following application of the [manipulative] technique resulted from treating the source of the pain.”
“Manipulative therapy [may] recruit the descending pain inhibitory system, through which it exerts a portion or all of its pain relieving effects. That is, manipulative therapy applied to the cervical spine produces a sensory input which could be sufficient to activate descending pain inhibitory system.”
“In a group of patients with lateral epicondylalgia, a manipulative therapy treatment technique applied to the lower cervical spine produced hypoalgesia at the elbow as manifest by increased pressure pain threshold, increased grip strength, improved neurodynamics and reduced pain over a 24 h period. This finding substantiates clinical observations that manipulative therapy is capable of producing improvements in pain and function immediately following application.”
Another study indicating that spinal manipulation is capable of activating the descending pain control system was published in the Journal of Back Musculoskeletal Rehabilitation in 2014, and titled (28):
The role of the Descending Inhibitory Pain Mechanism
in Musculoskeletal Pain Following High-Velocity,
Low Amplitude Thrust Manipulation: A Review of the Literature
The objective of this review was to investigate the role of the Descending Inhibitory Pain Mechanism in musculoskeletal pain following high-velocity, low amplitude thrust manipulation, as well as to identify the pain-relieving importance of this technique within clinical practice. The authors of this article make the following comments and conclusions:
“Although the antinociceptive effect of high-velocity, low amplitude thrust manipulation has been recognized by numerous systematic reviews, the underlying mechanism for manipulation-related pain relief remains poorly understood. An increasing number of studies have explored its analgesic mechanism suggesting that the excitation of the descending inhibitory pain mechanism might play the most important role for musculoskeletal pain relief.”
“Findings from current literature support that high-velocity, low amplitude thrust manipulation has a profound influence on nociceptive stimulus via the possible activation of the descending inhibitory pain mechanism. It seems that the application of this technique activates the periaqueductal gray region area of the midbrain, stimulates the noradrenergic descending system and at the level of the spinal cord, the nociceptive afferent barrage is reduced and mechanical hypoalgesia is induced.”
“The clinical importance of the activation of the descending inhibitory pain mechanism should not be ignored since the resulted analgesic effect of this technique can provide a window of opportunity to restore impaired physical performance and disability.”
Concluding Remarks
For decades, the periaqueductal gray matter descending pain inhibitory control system and their links to opiate receptors has been understood. Although it is proven that this descending pain control system can be activated with implanted electrodes, the inherent substantial and serious risks of such a procedure has minimized this approach.
As an alternative approach to activating this same system, opiate pharmacology has become the treatment of choice. However, this approach has resulted in a modern day epidemic and crisis, including receptor adaptation, addiction, substantial increased risk of heroin and other drug addiction, and death; side consequences include crime, destroyed families and incarceration; a social nightmare.
The evidence that chiropractic spinal adjusting can activate the descending pain control system, especially upper cervical chiropractic adjusting (29) is an important finding. Perhaps, all chronic pain patients should be evaluated and treated chiropractically for spinal biomechanical dysfunctions. Chiropractic has proven to be helpful in chronic pain patients with almost no risk to the patient.
REFERENCES
- Judy Foreman; A Nation in Pain; Healing Our Biggest Health Problem; Oxford University Press; 2014.
- Foreman J; Why Women are Living in the Discomfort Zone; More Then 100 Million American Adults Live with Chronic Pain—Most of them Women. What will it take to bring them relief?; January 31, 2014.
- Pho, K; USA TODAY, The Forum; September 19, 2011; pg. 9A.
- Wang S; Why Does Chronic Pain Hurt Some People More?; Wall Street Journal; October 7, 2013.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low Back Pain; Canadian Family Physician, March 1985, Vol. 31, pp. 535-540.
- Meade TW, Dyer S, Browne W, Townsend J, Frank OA; Low back pain of mechanical origin: Randomized comparison of chiropractic and hospital outpatient treatment; British Medical Journal; Volume 300, June 2, 1990, pp. 1431-7.
- Woodward MN, Cook JCH, Gargan MF, Bannister GC; Chiropractic treatment of chronic ‘whiplash’ injuries; Injury; Vol. 27; No. 9; November 1996; pp. 643-645.
- Khan S, Cook J, Gargan M, Bannister G; A symptomatic classification of whiplash injury and the implications for treatment; The Journal of Orthopaedic Medicine; Vol. 21; No. 1; 1999, pp. 22-25.
- Giles LGF, Muller R; Chronic Spinal Pain: A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation; Spine, July 15, 2003; 28(14):1490-1502.
- Muller R, Lynton G.F. Giles LGF, DC, PhD; Long-Term Follow-up of a Randomized Clinical Trial Assessing the Efficacy of Medication, Acupuncture, and Spinal Manipulation for Chronic Mechanical Spinal Pain Syndromes; Journal of Manipulative and Physiological Therapeutics, January 2005, Volume 28, No. 1.
- Kirkaldy-Willis WH, Managing Low Back Pain, Churchill Livingstone, 1983, p. 19.
- Cifuentes M, Willetts J, Wasiak R; Health Maintenance Care in Work-Related Low Back Pain and Its Association With Disability Recurrence; Journal of Occupational and Environmental Medicine; April 14, 2011; Vol. 53; No. 4; pp. 396-404.
- Senna MK, Machaly SA; Does Maintained Spinal Manipulation Therapy for Chronic Nonspecific Low Back Pain Result in Better Long-Term Outcome?
- Randomized Trial; SPINE; August 15, 2011; Volume 36, Number 18; pp. 1427–1437.
- Foreman SM, Croft AC; Whiplash injuries: The cervical acceleration/deceleration syndrome; 3rd Ed., Philadelphia: Lippincott Williams & Wilkins, 2002:525-526.
- Roger Chou, MD; Amir Qaseem, MD, PhD, MHA; Vincenza Snow, MD; Donald Casey, MD, MPH, MBA; J. Thomas Cross Jr., MD, MPH; Paul Shekelle, MD, PhD; and Douglas K. Owens, MD, MS; Diagnosis and Treatment of Low Back Pain; Annals of Internal Medicine; Volume 147, Number 7, October 2007, pp. 478-491.
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

