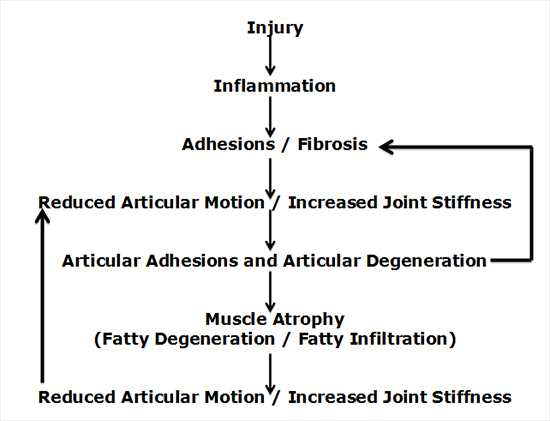
Tissue injury/trauma results in an inflammatory cascade (1, 2). This inflammatory cascade alters the threshold of the tissue nociceptors, which is why tissue injury is usually painful (3). The resolution of this inflammatory cascade is fibrosis/scar, a fibrous tissue response (4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14). This tissue fibrosis/scar will “limit the mobility of joints.” This concept is succinctly stated by Harvard Medical School professors Stanley Robbins, MD, and Ramzi Cotran, MD (7): “Reparative efforts may lead to disfiguring scars, fibrous bands that limit the mobility of joints.” Joints that lose motion degrade with adhesions, degenerative disease, and muscle atrophy, thereby creating deleterious feedback loops (15, 16, 17, 18, 19):
Specific citations for these concepts include: In 1981, The Journal of Orthopaedic and Sports Physical Therapy published a study titled (16):
Effects of Immobilization on the Extensibility of Periarticular Connective Tissue
This article discusses the biochemical and histological changes of periarticular connective tissue resulting from immobilization of synovial joints. The authors note:
“It is important for us to understand the nature of connective tissue and the histological changes that occur when connective tissue is immobilized. These changes are directly related to the causes of joint stiffness, leading to restricted movement.”
Immobilization of synovial joints causes “excessive connective tissue deposition in the joint and joint recesses. With time, this excessive fatty fibrous connective tissue formed a mature scar and created intra-articular adhesions.”
“With immobilization of synovial joints biochemical and histological changes occur within the periarticular connective tissue structures.” “Within the joint space and its recesses, there is excessive connective tissue deposition in the form of fatty fibrous infiltrate, which later matures to form scar tissue adhering to intra-articular surfaces further restricting motion.”
-
- In 1987, the journal Clinical Orthopedics and Related Researchpublished a study titled (18):
Connective Tissue and Immobilization: Key Factors in Musculoskeletal Degeneration?
The authors note:
“All situations that lead to immobilization can cause some degree of degenerative change in the musculoskeletal system.
When immobilization, whatever its cause, cannot be avoided, every attempt should be made to minimize it and to try to treat its harmful effects.”
-
- Another study was published in the journal Clinical Biomechanics in 1987 and titled (19):
Experimental Models of Osteoarthritis: The Role of Immobilization
The authors note:
“Immobilization, for whatever reason, is one of the pathogenic factors in musculo-skeletal degeneration.
It shows beyond reasonable doubt that immobilization is not only a cause of osteoarthritis but that it delays the healing process.”
••••••••••
Twenty-three years ago it was established that the structure most responsible for chronic whiplash neck pain is the facet joint capsular ligaments (20). Published in the journal Pain, the authors state:“A large proportion, if not the majority, of patients with post- traumatic neck pain have symptomatic zygapophysial joints.” In 2011, an important review article emphasizing the importance of the cervical spine facet joints in whiplash pain was published in the journal Spine, and titled (21):
On Cervical Zygapophysial Joint Pain After Whiplash
The author of the article, Nikolai Bogduk, MD, PhD, notes:
“There is convergent validity from (1) whiplash postmortem studies, (2) whiplash biomechanics studies, and (3) whiplash clinical studies indicating that the primary source of chronic whiplash pain is injuries to the cervical zygapophysial joints.”
“The fact that multiple lines of evidence, using independent techniques, consistently implicate the cervical zygapophysial joints as a site of injury and source of pain, strongly implicates injury to these joints as a common basis for chronic neck pain after whiplash.”
••••••••••
Two important issues pertaining to chronic whiplash/cervical facet joint pain are:
- Diagnosing it
- Predicting it in patients suffering from acute whiplash injury
For examples:
-
- In a 1994 study published in the journal Spine and titled (22):
Findings and Outcome in Whiplash-Type Neck Distortions
The authors assessed the clinical and imaging findings and late outcome in 50 patients with whiplash-type neck distortions 5 years after injury. Forty-eight percent of whiplash-injured patients have persistent pain at 5 years. The surgery revealed a high incidence of disco-ligamentous injuries in those with persistent pain. Importantly, these injuries could not be diagnosed with conventional imaging. The authors note that initial x-rays and MRIs are generally non-revealing as to the source of a whiplash-injured patient’s soft tissue injuries. They specifically state:
“Emergency radiograms are usually normal and may contribute to the physician’s perception of whiplash lesions as benign and self-limiting conditions.”
“Conventional radiograms are notoriously negative in whiplash-type injuries.”
“Magnetic resonance studies 6 to 8 weeks after the injury did not show any of the posterior injuries.”
-
- Nikolai Bogduk, in his article referenced above (21), notes:
“Medical imaging in vivo may fail to identify lesions that are definitely present at postmortem. Consequently, in the context of whiplash injury, normal radiographs, or even normal magnetic resonance imaging, do not mean that the patient has no lesion.”
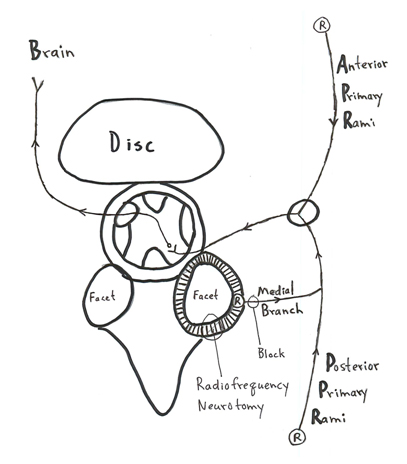
In this article, Dr. Bogduk further claims that these facet injuries and their chronic pain can only be diagnosed with invasive medial branch blocks of the posterior primary rami:
-
- In 2014, a study by Dr. Deniz Erbulut from Koc University School of Medicine in Istanbul, Turkey, published a study in the journal Turk Neurosurgery titled (23):
Biomechanics of Neck Injuries Resulting from Rear-End Vehicle Collisions
Dr. Erbulut agrees that the primary site of whiplash injury is the facet joint. However, he also notes:
X-rays and/or MRI have a limited ability to diagnose whiplash injuries. Whiplash injuries are “difficult to diagnose using methods such as basic radiography and MRI (Magnetic Resonance Imaging).”
••••••••••
New Understanding in the Diagnosis and Prognosis of Chronic Facet Whiplash Pain
New evidence has emerged suggesting that there is a non-invasive imaging way to diagnose chronic facet whiplash pain:
MRI Confirmed Fatty Infiltration of the Cervical Spine Multifidii Muscles
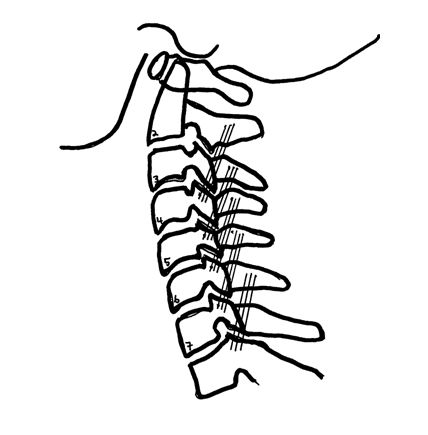
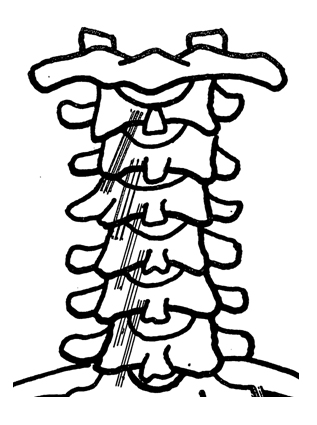
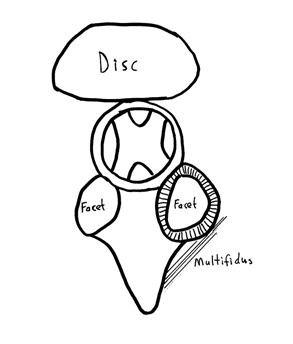
This approach is being championed primarily, but not exclusively, by Dr. James M. Elliott, PhD, PT, from the Department of Physical Therapy and Human Movement Sciences, Feinberg School of Medicine, Northwestern University, Chicago, IL (24, 25, 26). The cervical multifidus muscle originates on the articular process, extends cephalic and posterior-medial, inserting on the spinous process of the cervical vertebrae two levels above (see pictures). While ascending, they cross the posterior facet joint, reinforcing the posterior facet capsular ligaments. Consequently, it is biologically plausible that a whiplash injury to the facet joint would also injure the multifidii muscles.
A key study pertaining to whiplash multifidii injuries with fatty infiltration was published in 2015 in the journal Spine, and titled (26):
The Rapid and Progressive Degeneration of the Cervical Multifidus in Whiplash: A MRI study of Fatty Infiltration
In this study, Dr. James Elliott and colleagues add to the evidence that the fat/water content of the cervical spine multifidii muscles can be accurately assessed using standard MRI imaging. This study used 36 whiplash-injured subjects (Quebec Task Force Classification category of WAD Grade II), assessed at less than 1-week post-injury, 2-weeks post-injury, and 3-months post-injury. The authors were specifically looking for the temporal development of multifidii muscle fatty infiltrates (MFI) following whiplash, and the subject’s disability status. Subject disability status was measured with the Neck Disability Index (NDI), and classified as follows:
-
- 0–28% Recovered/Mild
- = 30% Severe
These authors cite that “half of all those exposed to a motor vehicle collision will never fully recover.” This study show that all subjects had essentially the same amount of multifidii muscle fatty infiltrates in the first exposed MRI (the one in the first week following their injury). However, in some patients, elevated and significant levels of multifidii fatty infiltration was observed in the 2nd week and 3 month MRI, indicating that some injured subjects experienced a significant and rapid fatty infiltration. Importantly, these subjects with the significant and rapid fatty infiltration are the same subjects who had severe disability and chronic pain at the 3-month assessment. Subjects who recovered from their injuries at 3 months did not have accelerating multifidii muscle fatty infiltration. These authors note:
“Multifidii muscle fatty infiltrate values were significantly higher in the severe group when compared to the recovered/mild group at 2-weeks and 3-months.”
“Comparing the recovered/mild to moderate/severe groups indicated no significant difference at 1 week with significant differences at 2 weeks and at 3 months.”
“While both groups entered the present study within one-week post-injury and had similar initial levels of MFI, the group with poor functional recovery uniquely demonstrated large muscle changes on water-fat MRI between 1- and 2-weeks post motor vehicle collision.”
“Conclusions—Consistent with previous evidence, muscle degeneration occurs soon after injury but only in those patients with poor functional recovery.”
Multifidii fatty infiltration is predictive for risk factors of developing chronic whiplash syndrome, and “routine imaging protocols may need to be reconsidered in the vast majority of patients following whiplash.”
[Routine MRI of the cervical spine, looking for multifidii MFI, may be necessary to predict whiplash chronicity].
“Multifidii fatty infiltration levels at 2 weeks may be used to predict severity based on NDI at 3 months.”
In this study, Dr. Elliott and colleagues propose mechanisms to account for the multifidii fatty infiltration and its associated poor recovery prognosis:
-
- The injury produced inflammation, resulting in disuse to minimize pain. Disuse of the muscles leads to atrophy and fatty infiltration. Elliott and colleagues state:
“Injury to a number of anatomical structures (facet joints, discs, ligaments, vascular tissues, and dorsal root ganglia) could produce an inflammatory response, which, similar to other chronic pain disorders, could affect the functioning of the peripheral and central nervous systems as well as the structure and strength of skeletal muscle.”
A logical approach to this mechanism is ice, low-level laser therapy, omega-3 fatty acids (fish oil), and controlled mobilization to disperse the accumulation of the inflammatory exudates. This controlled motion includes chiropractic spinal manipulation/adjusting.
-
- The whiplash event led to injury denervation of the medial branch of the spinal posterior primary rami, the nerve that innervates the multifidii muscles. Such neurological denervation reduces multifidii contractability, again leading to atrophy and fatty infiltration.
Denervated nerves will regenerate. A complication of this regeneration is the status of the muscle (multifidii) that was deprived of its nerve supply and its consequent atrophy and fatty infiltration. Conceptually, passive mobility, including chiropractic spinal manipulation (adjusting) will minimize such muscle atrophy and degeneration.
-
- The whiplash injury can result in increased sympathetic tone (27). Increased sympathetic tone can increase the tone in the associated muscles (28), leading to reduced motion, atrophy and fatty infiltration.
This is the classic neurophysiological description of the chiropractic subluxation (segmental articular dysfunction). Such dysfunctions are best managed with spinal manipulation (specific adjusting).
-
- Following whiplash injury, the patient may decrease activity and motion in an effort to minimize pain, resulting in atrophy and fatty infiltration. These authors state:
“The effect of depriving healthy individuals from their normal daily activity (as may be expected to occur if an individual reduces normal activity after a whiplash injury) can lead to fatigue, mood swings, reductions in muscle volume and intramuscular fatty infiltration.”
Encouraging the patient to remain engaged in normal activities as much as possible and to use their injured spines within the limits of pain should be a standard approach to managing these patients.
••••••••••
For decades, published studies have supported the use of controlled motion for the treatment of acute soft tissue injuries (1, 2, 8, 9, 11, 22, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39). This pertains to studies that specifically apply to whiplash injuries (40, 41). This also includes the use of chiropractic spinal manipulation for the treatment of chronic whiplash injury (42, 43). Perhaps these early motion techniques are preventing/minimizing the multifidii fatty infiltration notes above. As such, suggested management of whiplash injury should:
-
- Begin early, within a week of being injured.
- Encourage early and persistent movement.
- Employ early and persistent therapeutic movement, including exercise, passive articular movements, and chiropractic joint adjusting.
Additionally, especially in the early acute phases of injury, anti-inflammatory protocols seem logical, including ice, low-level laser therapy, omega-3s, etc.
REFERENCES
- Kellett J; Acute soft tissue injuries—a review of the literature; Medicine and Science in Sports and Exercise; October 1986; Vol. 18; No. 5; pp. 489-500.
- Russ A. Hauser RA, MD, E.E. Dolan EE, H.J. Phillips HJ, A.C. Newlin AC, Moore RE, Woldin BA; Ligament Injury and Healing: A Review of Current Clinical Diagnostics and Therapeutics; The Open Rehabilitation Journal; 2013; No. 6; pp. 1-20.
- Omoigui S; The biochemical origin of pain: The origin of all pain is inflammation and the inflammatory response: Inflammatory profile of pain syndromes; Medical Hypothesis; 2007; Vol. 69; pp. 1169–1178.
- Boyd W; PATHOLOGY: Structure and Function in Disease; Lea and Febiger, 1952.
- Boyd W; PATHOLOGY: Structure and Function in Disease; Eighth Edition; Lea & Febiger; Philadelphia; 1970.
- Anderson WAD, Scotti TM; Synopsis of Pathology; Ninth Edition; The CV Mosby Company; 1976.
- Robbins SL, Cotran RS; PATHOLOGIC BASIS OF DISEASE; Second Edition; WB Saunders Company; Philadelphia; 1979.
- Cyriax, James; Textbook of Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions; Bailliere Tindall; Volume 1; eighth edition; 1982.
- Roy, Steven; Irvin, Richard; Sports Medicine: Prevention, Evaluation, Management, and Rehabilitation; Prentice-Hall; 1983.
- Guyton A; Textbook of Medical Physiology; Saunders; 1986.
- Cohen, I. Kelman; Diegelmann, Robert F; Lindbald, William J; Wound Healing, Biochemical & Clinical Aspects; WB Saunders; 1992.
- Guido Manjo, MD and Isabelle Joris, PhD; Cells, Tissues, and Disease; Principles of General Pathology; Second Edition; Oxford University Press; 2004.
- Cailliet R; Soft Tissue Pain and Disability; 3rd Edition; F A Davis Company, 1996.
- Mehal WZ; Cells on Fire; Scientific American; June 2015; Vol. 312; No. 6; pp. 45-49.
- Langenskiöld A, Michelsson JE, Videman T; Osteoarthritis of the knee in the rabbit produced by immobilization. Attempts to achieve a reproducible model for studies on pathogenesis and therapy; Acta Orthopaedica Scandinvica; February 1979; Vol. 50; No. 1; pp. 1-14.
- Donatelli R, Owens-Brukhart H; Effects of Immobilization on the Extensibility of Periarticular Connective Tissue; The Journal of Orthopaedic and Sports Physical Therapy; Fall 1981; Vol. 3; No. 2; pp. 67-72.
- Videman T; Experimental osteoarthritis in the rabbit: comparison of different periods of repeated immobilization; Acta Orthopaedica Scandinvica; June 1982 Jun; Vol. 53; No. 3; pp. 339-47.
- Videman T; Connective tissue and immobilization. Key factors in musculoskeletal degeneration?; Clinical Orthopedics and Related Research; August 1987; Vol. 221; pp. 26-32.
- Videman T; Experimental models of osteoarthritis: the role of immobilization; Clinical Biomechanics; November 1987; Vol. 2; No. 4; pp. 223-9.
- Bogduk N, Aprill C; On the nature of neck pain, discography and cervical zygapophysial jointblocks; Pain; August 1993; Vol. 54; No. 2; pp. 13-17.
- Bogduk N;On Cervical Zygapophysial Joint Pain After Whiplash; Spine; December 1, 2011; Vol. 36; No. 25S, pp. S194–S199.
- Halldor Jonsson, Kristina Cesarini, Bo Sahlstedt, Wolfgang Rauschning; Findings and Outcome in Whiplash-Type Neck Distortions; Spine; December 15, 1994; Vol. 19; No. 24; pp. 2733-2743.
- Erbulut DU;Biomechanics of Neck Injuries Resulting fromRear-End Vehicle Collisions; Turk Neurosurgery; 2014; Vol. 24, No: 4; pp. 466-470.
- Elliott J, Pedler A, Kenardy J, Galloway G, Jull G, Sterling M. The temporal development of Fatty infiltrates in the neck muscles following whiplash injury: an association with pain and posttraumatic stress; PLoS One. 2011; 6(6):e21194.
- Abbott R, Pedler A, Sterling M, Hides J, Murphey T, Hoggarth M, Elliott J; The geography of fatty infiltrates within the cervical multifidus and semispinalis cervicis in individuals with chronic whiplash-associated disorders; Journal of Orthopedic and Sports Physical Therapy; April 2015; Vol. 45; No. 4; pp. 281-8.
- Elliott JM, Courtney DM, Rademaker A, Pinto D, Sterling, MM, Parrish TB; The Rapid and Progressive Degeneration of the Cervical Multifidus in Whiplash: A MRI study of Fatty Infiltration; Spine; June 15, 2015; Vol. 40; No. 12; pp. E694-E700.
- Passatore M, Roatta S; Influence of sympathetic nervous system on sensorimotor function: whiplash associated disorders (WAD) as a model; European Journal of Applied Physiology; November, 2006; Vol. 98; No. 5; pp. 423-449.
- Hubbard DR, Berkoff GM; Myofascial Trigger Points Show Spontaneous Needle EMG Activity; Spine; October 1, 1993; Vol. 18; No. 13; pp. 1803-1807.
- Stearns ML; Studies on development of connective tissue in transparent chambers in rabbit’s ear; American Journal of Anatomy; Vol. 67; 1940, p. 55.
- Seletz E; Whiplash Injuries, Neurophysiological Basis for Pain and Methods Used for Rehabilitation; Journal of the American Medical Association; November 29, 1958; pp. 1750–1755.
- Cyriax J; Textbook of Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions; Bailliere Tindall; Vol. 2; 1984.
- Frank C, Amiel D, Woo S, Akeson W; Normal ligament Properties and Ligament Healing; Clinical Orthopedics and Related Research; June, 1985; Vol. 196; pp. 15-25.
- Salter R, Continuous Passive Motion, A Biological Concept for the Healing and Regeneration of Articular Cartilage, Ligaments, and Tendons; From Origination to Research to Clinical Applications, Williams and Wilkins, 1993.
- Buckwalter J; Effects of Early Motion on Healing of Musculoskeletal Tissues; Hand Clinics; Vol. 12; No. 1; February 1996.
- Hildebrand K, Frank C; Scar Formation and Ligament Healing; Canadian Journal of Surgery; December 1998; Vol. 41; No. 6; pp. 425-429.
- Kannus P, Immobilization or Early Mobilization After an Acute Soft-Tissue Injury?; The Physician And Sports Medicine; March, 2000; Vol. 26 No 3, pp. 55-63.
- Hildebrand KA, Gallant-Behm CL, Kydd AS, Hart DA; The Basics of Soft Tissue Healing and General Factors that Influence Such Healing; Sports Medicine Arthroscopic Review September 2005; Vol. 13; No. 3; pp. 136–144.
- Schleip R; Fascia; The Tensional Network of the Human Body; The Scientific and Clinical Applications in Manual and Movement Therapy; Churchill Livingstone, 2012.
- Hauser RA, Dolan EE, Phillips HJ, Newlin AC, Moore RE, Woldin BA; Ligament Injury and Healing: A Review of Current Clinical Diagnostics and Therapeutics; The Open Rehabilitation Journal; 2013; No. 6; pp. 1-20.
- Mealy K, Brennan H, Fenelon GCC; Early mobilisation of acute whiplash injuries; British Medical Journal; March 8, 1986; Vol. 292; pp. 656-657.
- Rosenfeld M, Gunnarsson R, Borenstein P; Early Intervention in Whiplash-Associated Disorders; A Comparison of Two Treatment Protocols; Spine; July 15, 2000; Vol. 25; pp. 1782-1787.
- Woodward MN, Cook JCH, Gargan MF, Bannister GC; Chiropractic treatment of chronic ‘whiplash’ injuries; Injury; November 1996; Vol. 27, No. 9; pp. 643-645.
- Khan S, Cook J, Gargan MF, Bannister GC; A symptomatic classification of whiplash injury and the implications for treatment; The Journal of Orthopaedic Medicine; Vol. 21; No. 1; 1999, pp. 22-25.
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

