The cost of healthcare is extremely high in the United States. According to the California HealthCare Foundation, these are the most recent numbers (1):
United States Health Care Spending
|
2012 |
2014 (projected) |
|
|
Total Health Spending |
$2.8 Trillion |
$3.1 Trillion |
|
Health Care as |
17.2% |
18.3% |
|
Per CapitaSpending |
$8,915 |
$9,697 |
|
Growth in Total Spending |
3.0% |
5.2% |
In 2012 (the most recently available data), approximately 44% of the United States costs of Health Care were paid by government (Federal and State) agencies. This would amount to approximately $1.23 trillion.
This escalation in Health Care spending, especially by government agencies, has mandated an approach for cost containment, hopefully without compromising the quality of health care. The contemporary approach in this effort is called “Evidenced-Based Medicine.”
Evidence Based Medicine has been around for centuries, but its proponents have become increasingly organized in the 1990s. As an example, in 1996, the British Medical Journal published an editorial titled (2):
Evidence Based Medicine: What it is and What it isn’t
This article describes Evidence Based Medicine as:
“Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research.”
The accepted delivery of healthcare in the United States is increasingly becoming “Evidence Based.” A necessary component for the implementation of Evidence Based Medicine is the development and use of Clinical Practice Guidelines. As stated in the journal Health Affairs in 2005 (3):
“One common implementation of Evidence Based Medicine involves the use of clinical practice guidelines during medical decision making to encourage effective care.”
Evidence Based Medicine is not without criticism. A common criticism is that practice guidelines take the “doctoring” out of being a doctor. Doctors are increasingly being judged by Evidence Based Practice Guidelines. Doctors were (are) often questioned about their treatment approach to a particular patient when the approach varied from Evidence Based Practice Guidelines. Again, in 2005, the journal Health Affairs published a study titled (3) The Promises And Pitfalls Of Evidence-Based Medicine, which states:
“While advocates welcome the stronger scientific foundation of such guidelines, critics fear that they will lead to ‘cookbook medicine’.”
Another criticism of Evidence Based Practice Guidelines is that sometimes, “evidence” will “slip through the cracks.” As an example, apparently Evidence Based Practice Guidelines pertaining to the management of Low Back Pain, worldwide, advocate the use of the drug acetaminophen (the primary ingredient in Tylenol) as the first line treatment for acute low back pain. Astonishingly, this advice had never been subjected to the “gold standard” of evidence, the “double-blind, randomized controlled clinical trial.” Such a trial was completed last year, and published (November 1, 2014) in the journal The Lancet, and titled (4):
Efficacy of Paracetamol [Tylenol] for Acute Low-back Pain:
A Double-blind, Randomised Controlled Trial
The authors for this study are from the Sydney Medical School, Sydney, Australia. The study was a multicenter, double-blind, randomized, placebo controlled trial involving 1,652 patients with acute low-back pain. The authors made the following points:
- Low-back pain is the leading cause of disability worldwide.
- Guidelines for acute low-back pain universally recommend paracetamol [Tylenol] as the first-line analgesic; No direct evidence supports this universal recommendation.
- Regular paracetamol is the recommended first-line analgesic for acute low-back pain; however, no high-quality evidence supports this recommendation.
- There was no difference between treatment groups for time to recovery in this study.
“Our findings suggest that regular or as-needed dosing with paracetamol does not affect recovery time compared with placebo in low-back pain, and question the universal endorsement of paracetamol in this patient group.”
“Although guidelines endorse paracetamol for acute low-back pain, this recommendation is based on scarce evidence.”
“Neither regular nor as-needed paracetamol improved recovery time or pain intensity, disability, function, global change in symptoms, sleep, or quality of life at any stage during a 3- month follow up.”
The results of this study “suggest that simple analgesics such as paracetamol might not be of primary importance in the management of acute low-back pain, and the universal recommendation in clinical practice guidelines to provide paracetamol as a first-line treatment should be reconsidered.”
“Our results convey the need to reconsider the universal endorsement of paracetamol in clinical practice guidelines as first-line care for low-back pain.”
A follow-up Comment made in The Lancet pertaining to this study stated (5):
“Do patients with acute low-back pain need paracetamol?”
The findings of the Paracetamol for Low-Back Pain Study, show that paracetamol was not more effective than placebo in patients with acute low-back pain.
“In a well-designed and large clinical trial in Australia, 1652 patients with acute low-back pain were randomly assigned to receive paracetamol in regular doses, paracetamol as needed, or placebo.” The investigators reported no differences in the primary outcome (time to recovery) in any of the groups.
“Nor were differences recorded in secondary outcomes (eg, pain intensity, disability, symptom change, and function) between the three study groups.”
“This study is the first randomised clinical trial to assess paracetamol versus placebo for patients with acute low-back pain, and its results could have a substantial effect on the management of patients with low-back pain. Worldwide, national clinical guidelines recommend paracetamol as the first choice for prescribed analgesics for acute low-back pain.”
Evidence Based Guidelines for the chiropractic management of spinal problems began in 1992 with the publication of Guidelines for Chiropractic Quality Assurance and Practice Parameters: Proceedings of the Mercy Center Consensus Conference (6). These Guidelines are often referred to as the “Mercy Guidelines,” named after the location of the conference, the Mercy Conference Center in Burlingame, CA.
In 1989, the United States federal government established the Agency for Health Care Policy and Research. At that time the message was clear – either the health professions developed their own guidelines or third parties would impose them. The task of attempting to do something for the chiropractic profession was taken up by the Congress of Chiropractic State Associations or COCSA. Through a slow and detailed process, 35 chiropractors participated in developing a consensus document on chiropractic quality assurance and parameters of practice. The group had broad support from chiropractic colleges and organizations.
Despite being 23 years old, the Mercy Guidelines set the stage for more contemporary guidelines. The Mercy Guidelines make the following statements:
- “These recommendations do not give a ‘cookbook’ approach to the duration of care or number of treatments.”
- “They are NOT designed as a prescriptive or cookbook procedure for determining the absolute frequency and duration of treatment/care for any specific case.”
- “Note: statistical descriptions of treatment frequency such as mean/median/mode, should NOT be used as a standard to judge care administered to an INDIVIDUAL patient.”
Today, there are a number of guidelines for the management of spinal problems, including the recent, comprehensive, and authoritative Clinical Guidelines for the Diagnosis and Treatment of Low Back Pain that was published in the October 2007 issue of the journal Annals of Internal Medicine. An extensive panel of qualified experts constructed these clinical practice guidelines. These experts performed a review of the literature on the topic and then graded the validity of each study. The literature search for this guideline included studies from MEDLINE (1966 through November 2006), the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, and EMBASE. This project was commissioned as a joint effort of the American College of Physicians and the American Pain Society. The specific document pertaining to the chiropractic profession is titled (7):
Non-pharmacologic Therapies for Acute and Chronic Low Back Pain:
A Review of the Evidence for an American Pain Society
And American College of Physicians Clinical Practice Guideline
This article is probably the most comprehensive review of the literature concerning non-drug therapies used in the treatment of low back pain. It was prepared for the American Pain Society and the American College of Physicians Clinical Practice Guideline. These authors note that there are many non-pharmacologic therapies available for treatment of low back pain. They therefore assessed the benefits and harms of acupuncture, back schools, psychological therapies, exercise therapy, functional restoration, interdisciplinary therapy, massage, physical therapies (interferential therapy, low-level laser therapy, lumbar supports, shortwave diathermy, superficial heat, traction, transcutaneous electrical nerve stimulation, and ultrasonography), spinal manipulation, and yoga for acute or chronic low back pain (with or without leg pain). This article has 188 references.
Importantly, the Co-chairs and members of the American College of Physicians/American Pain Society Low Back Pain Guidelines Panel included one chiropractor, Donald R. Murphy, DC, DACAN.
The following chart summarizes the guideline’s recommendations for the treatment of acute, sub-acute, and chronic low back pain. Importantly, the only treatment approved for all three stages of low back pain is spinal manipulation.
The Following Chart Summarizes The Treatment Benefit For Low Back Pain
| Acute | Subacute | Chronic | |
| Manipulation | yes | yes | yes |
| Massage | insufficient | insufficient | yes |
| Acupuncture | no | no | yes |
| Exercise Therapy | no | no | yes |
| Yoga | no | no | yes |
| Back Schools | no | no | no |
| Psychological Therapies | no | no | no |
| Interdisciplinary Rehabilitation | no | no | yes |
| Interferential Therapy | no | no | no |
| Low-Level Laser Therapy | no | no | yes |
| Lumbar Supports | no | no | no |
| Shortwave Diathermy | no | no | no |
| Superficial Heat | yes | no | no |
| Traction | no | no | no |
| TENS | no | no | no |
| Ultrasound | no | no | no |
A central theme in Evidence Based Guidelines is that treatment should be reasonable and necessary. To establish that treatment is reasonable and necessary, the treating clinician should be using measurement outcomes.
Measurement Outcomes measure the health status of a patient before treatment, and then again after treatment (or a series of treatments) is/are performed. If the post treatment measurement outcome shows improvement, it is classically interpreted that the treatment was both reasonable and necessary. When measurement outcomes stop improving, it means that the patient’s clinical status has reached maximum improvement, or that a different clinical approach may be warranted.
There are literally hundreds of measurement outcomes available for health care providers. Each discipline of health care has developed recognized measurement outcomes that best serve their disciplines and patient’s needs. Chiropractors and other musculoskeletal disciplines often use the same measurement outcomes. These same measurement outcomes are often used in musculoskeletal research. For example, note:
- The number one ranked musculoskeletal journal in the world is the journal Spine. Spine is the official journal of publication for the world’s top thirteen orthopedic societies. In 2003, Spine published a study using the “gold standard” randomized clinical trial, comparing the benefits of prescription non-steroidal anti-inflammatory drugs (NSAIDs) to needle acupuncture to chiropractic spinal manipulation (adjusting) in patients suffering from chronic back and neck pain (8).
- The study evaluated patient progress using standard and accepted measurement outcomes:
- Oswestry Back Pain Disability Index (ODI)
- Neck Disability Index (NDI)
- Visual analog scales (VAS)
- Using these measurement outcomes, it was shown that needle acupuncture was twice as effective than the drugs in improving the patient’s pain and disability. Chiropractic spinal adjusting was better than five times more effective than the drugs. Also, importantly, only those receiving chiropractic spinal adjusting showed a long-term clinical benefit at the one-year follow-up assessment (9).
|
Drugs |
Acupuncture |
Chiropractic Adjustments |
|
|
Asymptomatic within 9 weeks |
5% |
9.4% |
27.3% |
Another research example using measurement outcomes is a study published in the journal Public Library of Science ONE (PloS One) in 2011 (10). The authors, from Harvard’s Medical School, used Positron Emission Tomography (PET) imaging to assess residual inflammation on patients suffering from chronic whiplash injuries. The authors used standard measurement outcomes to assess the patient’s clinical status:
- Neck Disability Index (NDI)
- Visual analog scales (VAS)
The authors showed that chronic whiplash patients do have regions of chronic inflammation that are consistent with their complaints, and that matched normal controls do not have these inflammatory regions. They conclude that their findings support an anatomical basis for chronic whiplash pain.
Clinically, measurement outcomes are primarily used for two purposes:
- To show that the treatment given was reasonable and necessary.
- To determine when the patients clinical status has reached maximum improvement.
Essentially, if measurement outcomes show progressive improvement in a patient’s clinical status, it means that the treatment given was reasonable and necessary, and that continued treatment is warranted. Additional treatment is warranted as long as the patient’s clinical status continues to improve.
In contrast, if measurement outcomes no longer show improvement, it is often interpreted as meaning that the patient’s clinical status had reached maximum improvement, and additional scheduled treatment may not be warranted. As an example, California chronic pain specialist, Jerome Schofferman, MD, used standard measurement outcomes to determine the recovery rate of people injured in motor vehicle accidents (11). Patients were treated until they became pain free, or until they reached maximum improvement, as assessed with measurement outcomes. Maximum improvement was determined to be when there was no significant change in symptoms and measurement outcomes for approximately 8 weeks.
Interestingly, the mean duration of treatment was 29 weeks (7 months 1 week); the range of treatment was 8 weeks (2 months) to 108 weeks (2 years and 1 month).
Secondary reasons to use measurement outcomes include:
- To document long-term or permanent symptoms and/or disabilities for a particular patient.
- To help apportion treatment, residual symptoms and permanent disabilities.
Reading the literature and a number of practice guidelines, the most important measurement outcomes for chiropractors are these:
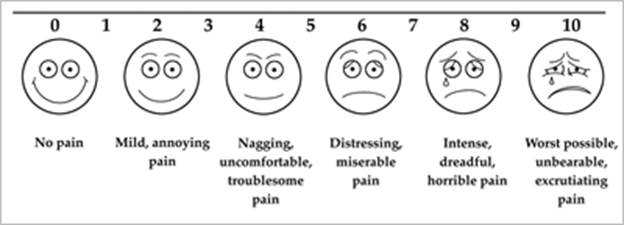
- Quantify the symptoms with the Visual Analog Scale (VAS).
- Use a standard Pain Drawing, ideally large enough for the patient to mark individual fingers and toes.
- The Oswestry Back Pain Disability Index (ODI).
- The Neck Disability Index (NDI).
- Samples of the Visual Analog Scale and Pain Drawing are attached.
- The frequency of the use of measurement outcomes is at the discretion of the treating doctor, but here are a few suggestions:
- All four of these should be used as a component of initial patient intake. The exception is that there is no need to do the Oswestry if the patient has no low back complaints, and there is no need to do the Neck Disability Index if the patient has no neck complaints.
- For patients under active care, these measurement outcomes should be completed at least once per month.
- For patients under maintenance care, these measurement outcomes should be completed at least once every 10-12 patient visits.
- At the discretion of the treating doctor, the Visual Analog Scale of the patient’s major symptoms may be done every visit.
- At the discretion of the treating doctor, the Pain Drawing may also be done every visit.
Measurement outcomes are now a standard component of contemporary clinical practice, including for chiropractors. Using measurement outcomes are an invaluable tool for the modern health care provider. Failure to use measurement outcomes invites criticism and conflict. Future health providers will be increasingly judged by their use of measurement outcomes and their results.
REFERENCES
- Wilson KB; Health Care Costs 101: US Health Care Spending; California HealthCare Foundation; www.chcf.org.
- Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WE; Editorials: Evidence based medicine: what it is and what it isn’t; British Medical Journal; January 13, 1996; 312:71.
- Timmermans S, Mauck A; The Promises And Pitfalls Of Evidence-Based Medicine; Health Affairs; January 2005; Vol. 24; No. 1; pp. 18-28.
- Williams CM, Maher CG, Latimer J, McLachlan AJ, Hancock MJ, Day RO, Lin CW; Efficacy of paracetamol for acute low-back pain: a double-blind, randomised controlled trial. Lancet. 2014 Nov 1;384(9954):1586-96.
- Koes BW, Enthoven WT; Do patients with acute low-back pain need paracetamol?; The Lancet; July 24, 2014 (published online).
- Haldeman S, Chapman-Smith D, Peterson DM; Guidelines for Chiropractic Quality Assurance and Practice Parameters: Proceedings of the Mercy Center Consensus Conference; Aspen publications; 1992.
- Chou R, Huffman LH; Non-pharmacologic Therapies for Acute and Chronic Low Back Pain: A Review of the Evidence for an American Pain Society And American College of Physicians Clinical Practice Guideline; Annals of Internal Medicine; October 2007, Volume 147, Number 7, pp. 492-504.
- Giles LGF, Muller R; Chronic Spinal Pain: A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation; Spine July 15, 2003; 28(14):1490-1502.
- Muller R, Giles LGF; Long-Term Follow-up of a Randomized Clinical Trial Assessing the Efficacy of Medication, Acupuncture, and Spinal Manipulation for Chronic Mechanical Spinal Pain Syndromes; Journal of Manipulative and Physiological Therapeutics; January 2005, Vol. 28; No. 1; pp. 3-11.
- Linnman C, Appel L, Fredrikson M, Gordh T, Soderlund A, Langstrom B, Engler H; Elevated [11C]-D-Deprenyl Uptake in Chronic Whiplash Associated Disorder Suggests Persistent Musculoskeletal Inflammation; Public Library of Medicine (PLoS) ONE; April 6, 2011, Vol. 6 No. 4, pp. e19182.
- Schofferman J, Wasserman S; Successful treatment of low back pain and neck pain after a motor vehicle accident despite litigation; Spine; May 1, 1994;19(9):1007-10.
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

