HISTORY:
Mandy, a 50-year-old female, was injured in a motor vehicle collision.
Her stationary vehicle was struck from the rear by a vehicle of similar mass that was traveling at a speed of approximately 20 miles per hour at the time of collision. Damage to her vehicle was judged to be $6,600.
The collision caught Mandy by surprise, and she was looking left at the moment of impact. This is important because there is good evidence (Sturzenegger 1994, Sturzenegger 1995) that factors associated with greater initial injury and a worse outcome one year after injury are (in descending order):
1) Being involved in a collision in which the patient is caught by surprise.
2) Being involved in a collision in which the patient’s head is rotated.
3) Being involved in a collision in which the impact is from a rear-end direction.
Although dazed, Mandy did not lose consciousness. An ambulance did take her to the emergency department of her own HMO, which was geographically close by.
At the hospital, Mandy was evaluated and radiographs were taken. There were no broken bones, signs of instability, congenital anomalies, or degenerative disease. She was told she had suffered a soft tissue injury and that it would get better in a few days to a few weeks.
For treatment, Mandy’s doctors put her into a soft cervical spine collar, she was prescribed a nonsteroidal anti-inflammatory drug, and given a heat pack for home use. She was advised to return for a follow-up visit if she was having continuing problems. Mandy was advised to continue to work in her usual occupation as a real estate agent.
Mandy began wearing her cervical spine soft collar most of the time. Although the anti-inflammatory medicines and the hot pack seemed to help her (this seems
paradoxical), she did not seem to be making overall relevant improvement. She continued to have significant neck pain and stiffness with an occasional headache.
Mandy did continue to work and actually missed no work at all. However, her neck was sore and stiff making her grumpy, and she became fatigued easily.
Mandy wore her cervical collar nearly constantly for about two weeks, then she reduced its usage to only when she was engaging in more strenuous activities, such as driving or shopping, and during certain activities at work. She liked her hot pack and she used it on average 3-4 times per day. She still needed her pain medicine, taking them a few times daily.
After about two months of being essentially unchanged, Mandy returned to her HMO physician and asked him if there was anything else she could do for her neck pain with occasional headaches. Her doctor authorized for Mandy to see one of the HMO’s physical therapists. She was prescribed one physical therapy session per week for the next four weeks.
Mandy’s physical therapist talked to her about her posture and gave her some exercises. He evaluated the ergonomics of her desk, primarily as related to when she was doing work on her computer.
After her four physical therapy visits, Mandy had incorporated his advice and exercises into her routine. Yet, she continued to suffer from neck pain and stiffness with occasional headaches.
Nine months after being injured, Mandy was still suffering and she could not go a full day without taking pain medications. Mandy needed to do something different.
Mandy became my patient nine months after being injured.
•••••
There is a common misconception that injured soft tissues will heal in a period of time between four and eight weeks. It is frequently claimed that injured soft tissues will heal spontaneously, leaving no long-term residuals, and that treatment is not required. This type of information is misleading and confusing because it is not true. As an example, in 2008, The American Journal of Medicine published a systemic review of the literature evaluating the clinical course of acute ankle sprain (Rijn 2008). The authors conducted a database search in MEDLINE, CINAHL, PEDro, EMBASE, and the Cochrane Controlled trial register. They found 31 studies that met their inclusion criteria. Their findings include:
- 5% to 33% of patients still experienced ankle pain after 1 year.
- The studies reported an incidence of subjective instability of their injured ankle in up to 53% patients.
- 15% to 64% had not fully recovered at 3 years.
- The incidence of re-sprains ranged from 3% to 34% of the patients.
Most of my med-legal experience is with whiplash injury. Often, insurance defense personnel and their chiropractic/medical experts make an analogy between the whiplash-injured neck and a sprained ankle. Their classic claim is that a sprained ankle will heal spontaneously (without any treatment) and quickly (weeks), and there are no long-term residuals.
This article by Rijn presents a much different reality pertaining to the healing of the sprained ankle: at 3 years up to 64% have not fully recovered, up to 33% have residual pain, up to 53% suffer from residual instability, and up to 34% suffer from re-injury. It appears that 15% to 64% have some degree of permanent injury. Additionally, the severity of ankle injury is not a strong predictor for the ultimate clinical outcome. It appears that trauma from ankle sprain and whiplash have a number of shared characteristics: significant residual pain, instability, re-injury rates, permanent injury residuals, and the severity of injury not being a predictor for the ultimate clinical outcome.
Consequently, I believe that the most important question is:
Is there an approach to the management of injured soft tissues that improves the timing and quality of the healing outcome?
•••••
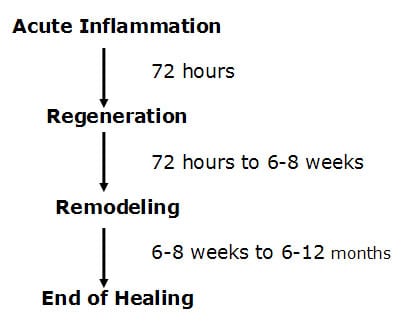
Published articles and books concerning the healing of injured soft tissues (Oakes 1982; Roy and Irving 1983; Kellett 1986; Buckwalter/Woo 1988, Majno 2004) indicate that the time frame for soft healing is approximately one year.
The healing of injured soft tissues takes place in three specific phases. The first phase is called the acute inflammatory phase. This phase will last approximately 72 hours. During this phase, after the initial injury, an electrical current is generated at the wound, called the “current of injury.” This “current of injury” attracts fibroblasts to the wound (Oschman, 2000). During this phase there is also initial bleeding and continual associated inflammation of the injured tissues. Because of the increasing inflammatory cascade during this period of time, it is not uncommon for the patient to feel worse for each of the first three days following injury. Because there is disruption of local vascular supplies, there is insufficient availability of substrate (glucose,
oxygen, etc.) to produce large enough quantities of ATP energy to initiate collagen protein synthesis to repair the wound.
Experience and published studies (Kellett 1996) indicate that the best management of soft tissue injuries during the acute inflammatory phase is ice therapy. Ice therapy during the first 72 hours following injury reduces pain and swelling, and minimizes the formation of scar tissue that often causes prolonged disability (Seletz 1958). [Unfortunately for Mandy, during this phase of soft tissue healing, she was prescribed and used heat].
After 72 hours following injury, the damaged blood vessels have mended. The resulting increased availability of glucose and oxygen elevates local ATP levels and collagen repair begins by the fibroblasts that accumulated during the acute inflammatory phase. This second phase of healing is called the phase of regeneration. During the regeneration phase the disruption in the injured muscles and ligaments is bridged. Some references call the regeneration phase the phase of repair, which creates confusion about the timing of healing (Jackson, 1977). “Repair” connotation is that the process has completed, which, as we will see, is not the case. The fibroblasts manufacture and secrete collagen protein glues that bridge the gap in the torn tissues. This phase will last approximately 6-8 weeks (Jackson, 1977). At the end of 6-8 weeks, the gap in the torn tissues is more than 90% bridged; more than 90% of the collagen that is laid down in the breach occurs during this second phase of healing. Consequently, many will erroneously claim this to be the end of healing. However, it clearly is not.
Experience and published studies (Stearns 1940, Seletz 1958, Cyriax 1982, Roy 1983, Kellett 1986, Mealy 1986, Cohen 1992, Salter 1993, Jonsson 1994, Buckwalter 1996, Kannus 2000, Rosenfeld 2000) document that the best management of soft tissue injuries during the second phase of healing is early, persistent, controlled mobilization. In contrast, immobilization is harmful, leading to increased risk of slowed healing and chronicity (Stearns 1940, Mealy 1986, Cohen 1992, Salter 1993, Jonsson 1994, Kannus 2000, Rosenfeld 2000, Schofferman 2007). [Unfortunately for Mandy, during this second phase of soft tissue healing, she was prescribed and used a cervical collar].
There is a third and final phase of healing. This phase is called the phase of remodeling.
The phase of remodeling starts near the end of the phase of regeneration. During the phase of remodeling the collagen protein glues that have been laid down for repair are remodeled in the direction of stress and strain. This means that the fibers in the tissue will become stronger, and will change their orientation from an irregular pattern to a more regular pattern, a pattern more like the original undamaged tissues. Proper treatment during this remodeling phase is very necessary if the tissues are to get the best end product of healing. It is during this remodeling
phase that the tissues regain strength and alignment. Remodeling takes approximately one year from the date of injury. It is established that remodeling takes place as a direct byproduct of motion. Chiropractic healthcare puts motion into the tissues in an effort at getting them to line up along the directions of stress and strain, thereby giving a stronger, more elastic end product of healing.
Stages of Healing Following Soft Tissue Injury
Possible Residual Fibrotic Changes
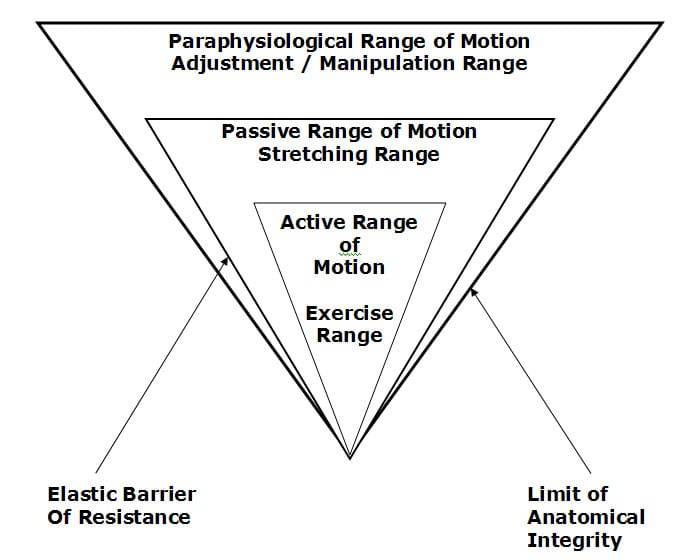
Traditional chiropractic joint manipulation healthcare is directed towards putting motion into the periarticular paraphysiological space. The concept of paraphysiological joint motion was first described by Sandoz in 1976, and is explained well by Kirkaldy-Willis 1983 and 1988, by Kirkaldy-Willis/Cassidy 1985, and in the 2004 monograph on Neck Pain (edited by Fischgrund) published by the American Academy of Orthopedic Surgeons (see picture). These discussions clearly show that there is a component of motion that cannot be properly addressed by exercise, massage, etc., and that this component of motion can be properly addressed by osseous joint manipulation. Therefore, traditional chiropractic osseous joint manipulation adds a unique aspect to the treatment and the remodeling of periarticular soft tissues that have sustained an injury.
During this third phase of healing, the phase of remodeling, Mandy continued to wear a cervical collar, especially during high-demand activities. Although she did add some exercises to her management, which is helpful, she employed no management aspects that would have introduced motion into the periarticular paraphysiological
space. As Schofferman and Bogduk state in their 2007 article titled: Chronic whiplash and whiplash-associated disorders: An evidence-based approach,
“exercise alone is rarely curative”
Additionally, Drs. Schofferman and Bogduk suggest there is value in spinal manipulation in the management of chronic whiplash patients (Schofferman, 2007).
•••••
Mandy’s whiplash soft tissue injury management that included heat, immobilization and limited exercises did not result in an acceptable clinical outcome. Nine months after being injured, she was suffering from chronic neck pain, weakness, and occasional headaches.
My approach to her management included:
- Regular and strenuous resistive effort exercises of the muscles of her cervical and thoracic spines.
- No more use of a cervical collar.
- Transverse friction myotherapy to reduce the adverseness of post-traumatic muscular adhesions and fibrosis (Cyriax, 1982).
- Specific osseous joint manipulation to the joints that were reduced in the symmetry and/or magnitude of normal motion. Such manipulations will reduce articular adhesions, remodel periarticular fibrosis, reduce muscle hypertonicity and spasm, and close the “pain gate” (Kirkaldy-Willis, 1983, 1985, 1988).
- Specific chiropractic postural correctional techniques. Improved posture reduces stresses in both soft tissues, muscles, and articulations.
Mandy remained under my care for a period of 4 months, and she was seen a total of 32 visits at our clinic. Her progress was steady and progressive. When she was released from additional regularly scheduled treatment, she was instructed to continue to do her prescribed exercises. Mandy’s symptoms were not completely resolved, but she judged her clinical status to be 85% improved as compared to when she first entered our clinic.
•••••
There are some problems associated with the healing of injured soft tissues. Microscopic histological studies show that the repaired tissue is different than the original, adjacent, undamaged tissues. During the initial acute inflammatory phase there is bleeding from the damaged tissues and consequent local inflammation. This progressive bleeding releases increased numbers of fibroblasts into the surrounding tissues. Chemicals that are released trigger the inflammation response that is noted in cases of trauma. Subsequent to the inflammatory response and to the number of fibrocytes that are released into the tissues, the healing process is really a process of fibrosis. In 1975, Stonebrink addresses that the last phase of the pathophysiological response to trauma is tissue fibrosis. Boyd in 1953, Cyriax in 1983, and Majno/Joris in 2004 note that there is tissue fibrosis subsequent to trauma. This fibrosis of repair subsequent to soft tissue trauma creates problems that can adversely affect the tissues and the patient for years, decades, or even forever.
Fibrosed tissues are functionally different from the adjacent normal tissues. The differences fall into two main categories:
Category 1: The repaired tissue is weaker and less strong than the undamaged tissues. This is because the diameter of the healing collagen fibers are smaller, and the end product of healing is deficient in the number of crossed linkages within the collagen repair.
Category 2: The repaired tissue is stiffer or less elastic than the original, undamaged tissues. This is because the healing fibers are not aligned identically to that of the original. Examination range of motion studies will indicate that there are areas of decrease of the normal joint ranges of motion.
In addition, Cyriax notes “fibrous tissue is capable of maintaining an inflammatory response long after the initial cause has ceased to operate.” Since inflammation alters the thresholds of the nociceptive afferent system (Omoigui 2007), physical examinations in these cases will show these fibrotic areas display increased sensitivity, and digital pressure may show hypertonicity and spasm. This increased sensitivity can be documented with the use of an algometer, which is a device that uses pressure to determine the initiating threshold of pain.
Because the fibrotic residuals have rendered the tissues weaker, less elastic, and more sensitive, the patient will have a history of flare-ups of pain and/or spasm at times of increased use or stress. These episodes of pain and/or spasm at times of increased use or stress of the once damaged soft tissues is the rule rather than the exception, and a problem that the patient will have to learn to live with. It is likely that the patient will continue to have episodes of pain and/or spasm for an indefinite period of time in the future. It is probable that the patient will have a need for continuing care subsequent to these episodes of pain and/or spasm.
Consistent with these concepts, a study by Hodgson in 1989 indicated that 62% of those injured in automobile accidents still have significant symptoms caused by the accident 12 1/2 years after being injured; and that of the symptomatic 62%, 62.5% had to permanently alter their work activities and 44% had to permanently alter their
leisure activities in order to avoid exacerbation of symptoms. One of the conclusions of the article is that these long-term residuals were most likely the result of post-traumatic alterations in the once damaged tissues.
A study by Gargan in 1990 indicated that only 12% of those sustaining a soft tissue neck injury had achieved a complete recovery more than ten years after the date of the accident. One of the conclusions of this study is that the patient’s symptoms would not improve after a period of two years following the injury.
It is established neurologically (Wyke 1985, Kirkaldy-Willis and Cassidy 1985) that when a chiropractor adjusts (specific directional spinal manipulation) the joints in the region of pain and/or spasm, that there is a depolarization of the mechanoreceptors that are located in the facet joint capsular ligaments, and that the cycle of pain and/or spasm can be neurologically aborted. This is why many patients feel better after they receive specific joint manipulation from a chiropractor following an episode of increased pain and/or spasm.
What is the basis for the chronic post-trauma pain syndromes that so many patients suffer from? A good explanation is found from Gunn (1978, 1980, 1989). He refers to this type of pain as supersensitivity. The supersensitivity type pain is a residual of the scarring or the fibrosis that was created by the injuries sustained in this accident. The treatment that we give to the patient for the injuries sustained in an accident is really not designed to heal the sprain or strain but rather, to change the fibrotic nature of the reparative process that has left the patient with residuals that are weaker, stiffer, and more sore. The actual diagnosis for this type of problem is initial sprain/strain injuries of the paraspinal soft tissues with fibrotic residuals subsequent to the fibrosis of repair of once damaged soft tissues that have left these tissues weaker, stiffer, and more sensitive as compared to the original tissues. The majority of our efforts in the treatment of post-traumatic chronic pain syndrome patients is in dealing with the residual fibrosis of repair and its associated mechanical and neurological consequences. These residuals to some degree are most probably permanent. The patient will have to learn to deal with the long-term residuals and the occasional episodes of pain and/or spasm. However, as noted above, occasional specific joint manipulation in the involved areas can neurologically inhibit muscle tone, improve ranges of motion, disperse accumulated inflammatory exudates, and the patient will have less pain and improved function.
The concepts briefly discussed above are frequently not understood or appreciated. There is a tendency for healthcare providers to not properly examine the patient in order to document these regions of tissue fibrosis and its consequent mechanical and neurological consequences and, therefore, to quote Stonebrink, the real problem is missed.
•••••
I believe that for Mandy, her poor early management resulted in excessive tissue fibrosis, and as noted above, that was the basis for her chronicity. Our management of her problems reduced the magnitude of her fibrotic residuals and their adverseness. Her cervical spine range of motion increased, her posture improved, her muscle strength increased and her musculoskeletal fatigue resolved. She no longer used her cervical collar and she did not need any pain medications. Her residual symptoms were manageable and tolerable with continuing cervical spine exercise. It is probable that some of her fibrotic residuals were not reducible, creating the pathoanatomical basis for her residual symptoms (Josson 1994).
Addendum
Three months after Mandy was released from treatment, she was involved in another similar motor vehicle collision. She sustained significant soft tissue injuries of her cervical and thoracic spines, essentially in the exact locations of the collision she had sustained approximately nineteen months prior.
The day of this second injury, Mandy presented herself to our clinic for management.
Our acute care protocol included recumbent traction (for 20 minutes) with a cervical pillow and ice pack. This was done four times per day, once in the office and three times at home. She was initially seen in our office daily for the first three weeks following her injury. Low-level laser therapy was applied for 20 minutes daily to her injured spinal regions in an effort to elevate ATP levels, accelerating the healing process.
On the fourth day, we added to her management a passive motion protocol to the joints of the cervical and thoracic spines; each of her joints were carefully pushed into the passive range of motion (see picture below) while using the laser with an anti-inflammatory setting. This is done in an effort to disperse inflammation and thereby reduce long-term scarring (fibrosis). It also puts tension in the developing granulation tissue, improving alignment and strength. This is a benefit that cannot be achieved by exercise alone.
At two weeks, we began to provide specific joint manipulation (adjustments) to the articulations that showed reduced and/or altered motion patterns. Simultaneously, postural corrections, transverse friction myotherapy and resistive effort exercises were initiated.
Mandy’s entire trauma management program lasted eighteen weeks; she was seen in our office a total of 34 times. When she was released from additional regularly scheduled treatment, she reported to be 100% resolved of all signs and symptoms. This means that the residuals she had from her prior accident had completely resolved. I believe that the second accident had re-torn the fibrotic residuals she retained from her prior collision. The magnitude of the second collision was such that
it reduced fibrotic residuals that I was unable to reduce therapeutically. But I now had the opportunity to manage her new acute injuries with a different, superior approach. The results were gratifying for both Mandy and myself.
Joint Ranges of Motion
REFERENCES
Boyd, William, M.D., Pathology, Lea & Febiger, (1952).
Buckwalter J, Effects of Early Motion on Healing of Musculoskeletal Tissues, Hand Clinics, Volume 12, Number 1, February 1996.
Cohen, I. Kelman; Diegelmann, Robert F; Lindbald, William J; Wound Healing, Biochemical & Clinical Aspects, WB Saunders, 1992.
Cyriax, James, M.D., Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions, Bailliere Tindall, Vol. 1, (1982).
Fischgrund, Jeffrey S, Neck Pain, monograph 27, American Academy of Orthopaedic Surgeons, 2004.
Gargan, MF, Bannister, GC, Long-Term Prognosis of Soft-Tissue Injuries of the Neck, Journal of Bone and Joint Surgery, September, 1990.
Gunn, C. Chan, Pain, Acupuncture & Related Subjects, C. Chan Gunn, (1985).
Gunn, C. Chan, Treating Myofascial Pain: Intramuscular Stimulation (IMS) for Myofascial Pain Syndromes of Neuropathic Origin, University of Washington, 1989.
Hodgson, S.P. and Grundy, M., Whiplash Injuries: Their Long-term Prognosis and Its Relationship to Compensation, Neuro-Orthopedics, (1989), 7.88-91.
Jonsson H, Cesarini K, Sahlstedt B, Rauschning W, Findings and Outcome in Whiplash-Type Neck Distortions; Spine, Vol. 19, No. 24, December 15, 1994, pp. 2733-2743.
Kannus P, Immobilization or Early Mobilization After an Acute Soft-Tissue Injury?; The Physician And Sports Medicine; March, 2000; Vol. 26 No 3, pp. 55-63.
Kellett J; Acute soft tissue injuries-a review of the literature; Medicine and Science of Sports and Exercise, American College of Sports Medicine, Vol. 18 No.5, (1986), pp. 489-500.
Kirkaldy-Willis, W.H., M.D., Managing Low Back Pain, Churchill Livingston, (1983 & 1988).
Kirkaldy-Willis, W.H., M.D., & Cassidy, J.D.,“Spinal Manipulation in the Treatment of Low-Back Pain,” Can Fam Physician, (1985), 31:535-40.
Majno, Guido and Joris, Isabelle, Cells, Tissues, and Disease: Principles of General Pathology, Oxford University Press, 2004.
Mealy K, Brennan H, Fenelon GCC; Early Mobilization of Acute Whiplash Injuries; British Medical Journal, March 8, 1986, 292(6521): 656-657.
Oakes BW. Acute soft tissue injuries. Australian Family Physician. 1982; 10 (7): 3-16.
Omoigui S; The biochemical origin of pain: The origin of all pain is inflammation and the inflammatory response: Inflammatory profile of pain syndromes; Medical Hypothesis; 2007, Vol. 69, pp. 1169-1178.
Oschman, James L, Energy Medicine: The Scientific Basis, Churchill Livingstone, 2000.
Rogier M. van Rijn, Anton G. van Os, Roos M.D. Bernsen, Pim A. Luijsterburg, Bart W. Koes, Professor, Sita M.A. Bierma-Zeinstra; What Is the Clinical Course of Acute Ankle Sprains? A Systematic Literature Review; The American Journal of Medicine; April 2008, Vol. 121, No. 4, pp. 324-331.
Rosenfeld M, Gunnarsson R, Borenstein P, Early Intervention in Whiplash-Associated Disorders, A Comparison of Two Treatment Protocols; Spine, 2000;25:1782-1787.
Roy, Steven, M.D., and Irvin, Richard, Sports Medicine: Prevention, Evaluation, Management, and Rehabilitation, Prentice-Hall, Inc. (1983).
Salter R, Continuous Passive Motion, A Biological Concept for the Healing and Regeneration of Articular Cartilage, Ligaments, and Tendons; From Origination to Research to Clinical Applications, Williams and Wilkins, 1993.
Seletz E; Whiplash Injuries; Neurophysiological Basis for Pain and Methods Used for Rehabilitation; Journal of the American Medical Association; November 29, 1958, pp. 1750-1755.
Schofferman J, Bogduk N, Slosar P; Chronic whiplash and whiplash-associated disorders: An evidence-based approach; Journal of the American Academy of Orthopedic Surgeons; October 2007;15(10):596-606.
Stonebrink, R.D., D.C., “Physiotherapy Guidelines for the Chiropractic Profession,” ACA Journal of Chiropractic, (June1975), Vol. IX, p.65-75.
Stearns, ML, Studies on development of connective tissue in transparent chambers in rabbit’s ear; American Journal of Anatomy, vol. 67, 1940, p. 55.
Sturzenegger M, DiStefano G, Radanov BP, Schnidrig A. Presenting symptoms and signs after whiplash injury: the influence of accident mechanisms. Neurology. April 1994;44(4):688-93.
Sturzenegger M, Radanov BP, Di Stefano G. The effect of accident mechanisms and initial findings on the long-term course of whiplash injury. Journal of Neurology. July 1995;242(7):443-9.
Wyke, B.D., Articular neurology and manipulative therapy, Aspects of Manipulative Therapy, Churchill Livingstone, 1980, pp.72-77.
Woo, Savio L.-Y.,(ed.), Injury and Repair of the Musculoskeletal Soft Tissues, American Academy of Orthopaedic Surgeons,(1988), p.18-21; 106-117; 151-7; 199-200; 245-6; 300-19; 436-7; 451-2; 474-6.
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

