From the earliest moments of his life, Joe was an extremely active boy. He would attempt to climb up on to everything he could, often falling off: furniture, vehicles, rocks, trees, etc. When he began school, he was constantly involved in every sport available to him: football, baseball, basketball, soccer, gymnastics, and more. Joe particularly like the rougher sports, like football; the rougher the sport the more Joe enjoyed it.
Joe was raised a practicing Catholic. Catholic church services (mass), includes periods of kneeling down. Joe’s earliest memories of kneeling during mass are that of having low back pain. Kneeling put his lumbar spine in a slightly extended, increased lordotic, position. Joe’s back felt much better if he would move his butt back until it contacted the seat behind him, putting him in a semi seated-kneeling position. In this position his lumbar spine was in slight flexion, and his back did not hurt. However, Joe’s parents felt that assuming such a position was disrespectful, and they would regularly gently reminded him to straighten up.
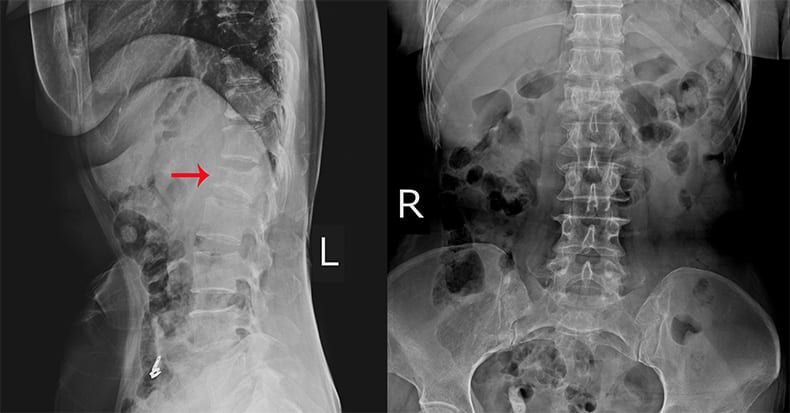
In high school, Joe excelled in football, basketball, and track. In track he did it all, competing in all the events of the decathlon. In college, Joe played basketball and ran on the track team. But during his college sophomore year he began to experience chronic lower back pain. Eventually he saw a chiropractor for his chronic low back pain complaints. The chiropractic examination included upright lumbar spine radiographs. The initial working diagnosis was:
Spondylolysis with spondylolisthesis (grade II, a 50% forward slippage down the sacral base) resulting in moderate L5-S1 disc degeneration (spondylosis) and paravertebral muscle spasm. There was no radiculopathy or myelopathy.
•••••••••
In the reference text The Physiology of the Joints, former Chief of Clinical Surgery at the Hospital of Paris, IA Kapandji, states:
“The lumbo-sacral joint is the weak link in the vertebral column.”
Dr. Kapandji’s explanation for this statement is likened to the proverbial physics of a block on an incline plane. When a block is on an inclined plane, the vertical force of gravity (G) is broken into two vectors:
C: A compression component
S: A sheer component
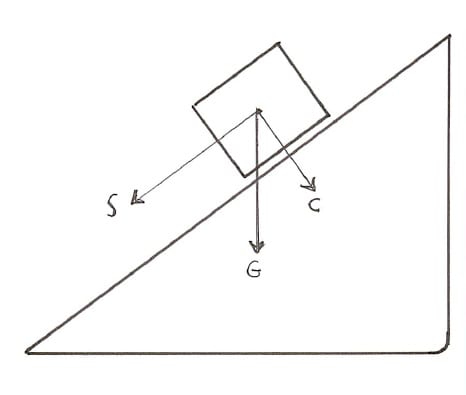
As Dr. Kapandji explains, the sacral base is not horizontal, but rather it is an inclined plane. The L5 vertebral body sits atop of the inclined plane of the sacral base. The main structure that prevents the L5 vertebral body from sliding anterior and inferior down the sacral base inclined plane is the posterior vertebral arch (vertebral isthmus). This vertebral isthmus exists between the superior and inferior facets of L5, a location that is known as the pars interarticularis.
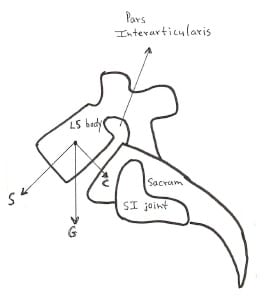
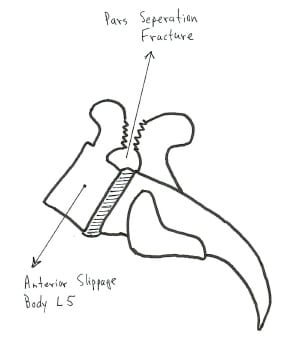
The fracture and separation of the pars interarticularis is known as spondylolysis. When the pars is fractured or destroyed, the L5 vertebral body will slide down the incline plane of the sacral base. This anterior and inferior slippage of the L5 vertebral body is known as an anterior spondylolisthesis.
Dr. Kapandji notes that when the pars is separated, the remaining structures that resist the slippage of the L5 disc down the sacral inclined plane are the fibers of the intervertebral disc and the posterior paraspinal musculature. The mechanical stress on the annular fibers of the L5 intervertebral disc can generate discogenic low back pain. The constant contraction and spasm of the posterior paraspinal musculature can cause muscular low back pain.
•••••••••
Congenital or Acquired
Incidence, Location, and Onset of Symptoms
Up until the 1970s it was commonly thought and taught that spondylolysis and anterior spondylolisthesis were congenital. However, autopsies on stillborn babies and careful analysis of adults who had never walked indicated that spondylolysis and anterior spondylolisthesis are not congenital. For decades now, it has been understood that spondylolysis and anterior spondylolisthesis are acquired in childhood. A chronological review of the evidence include these:
- In 1965, Melamed publishes an article titled:
SPONDYLOLYSIS AND SPONDYLOLISTHESIS ARE NOT CONGENITAL
- In 1971, Schmoral and Junghanns note:
There is increasing support for the opinion that spondylolysis is “acquired after birth during growth of the skeletal system.” Spondylolysis “seems to be closely connected to the upright gait and to the lumbar lordosis.”
- In 1973, Farfan notes:
Evidence “suggests that the defect in the neural arch is acquired,” and that the “condition is a stress fracture.”
- In 1975, Cyriax notes:
“Evidence has lately been accumulati ngthat a disorder named spondylolisthesis (which had been regarded as due to an inborn defect in the vertebral arch) is seldom congenital but is acquired in childhood.”
“Stress fractures form between the two halves of the vertebral arch.”
- In 1977, Mcnab notes:
“In spondylolytic spondylolisthesis, the basic lesion is a defect in the neural arch across the pars interarticularis.” “The neural arch defects occur most frequently between ages of 5 and 7. Forward slippage of the vertebral body occurs most frequently between ages of 10 and 15 and rarely increases after 20.”
“In some Eskimo communities the incidence of neural arch defects may rise as high as 50%.” “The incidence of spondylolysis in the white population of the North American continent is about 6%.”
- In 1977, D’Ambrosia notes:
Spondylolysis with spondylolisthesis “only occurs in man who walks with a true upright stance and has lumbar lordosis. There is no evidence that this defect is ever present at birth, and it is not seen in patients who have never been ambulatory. The most common age of onset is between 5 and 6 years of age, but slipping can occur up to age 20. The period of most rapid slipping is between 10 and 15 years when the adolescent growth spurt is at its peak.”
- In 1980, Keim notes:
“Many authorities consider spondylolysis and spondylolisthesis to be stress fractures of the pars interarticularis, or isthmus, of a vertebrae.”
“After the age of 5 and usually in the teenage years, repeated shearing stresses, such as those that occur in gymnastics or contact sports, can cause a stress fracture in the isthmus.”
- In 1980, Finneson notes:
Spondylotic spondylolisthesis is due to a separation or dissolution of the pars. “It is always a fatigue fracture.” It is almost never seen below the age of 5, but is found in 4.4% of 7 year olds.
- In 1980, Wertzberger and Peterson note:
“There is increasing evidence that the defect in the pars interarticularis is due to fatigue fracture rather than being of congenital origin. We describe the youngest patient on record with spondylolysis and spondylolisthesis in whom roentgenograms that showed no abnormality had previously been taken. This case supports the hypothesis that spondylolysis and spondylolisthesis are acquired and not congenital, even when discovered in a very young child.”
- In 1981, Rosenberg and colleagues obtained radiographs of the lumbosacral spines of 143 patients (age range of 11 to 93 years) that had never walked. They note:
“No case of spondylolysis or spondylolisthesis was detected, and when compared to the 5.8% incidence in the general population.”
“These results support the theory that spondylolysis and isthmic spondylolisthesis represent a fatigue fracture resulting from activities associated with ambulation.”
- In 1983, Salter notes:
Approximately 85% of spondylolysis “occur in the fifth lumbar vertebrae and most of the remaining 15% occur in the fourth lumbar vertebrae.”
“Once thought to be a congenital defect spondylolysis is now known to develop during postnatal life.”
“Since the lower lumbar region of the human spine is subjected to much stress in the erect position, it is possible that spondylolysis represents either a stress fracture (fatigue fracture) from oft-repeated stresses or an ordinary fracture from a single injury.”
The gap in the pars after fracture and separation is filled in with fibrous tissue.
“The forward slippage of one vertebral body (and the remainder of the spinal column above it) in relation to the vertebral segment immediately below is referred to as a spondylolisthesis. It occurs most commonly in the lower lumbar spine—particularly between the fifth lumbar vertebrae and the sacrum.”
A normal lumbar vertebral body is prevented from slipping forward by an intact neural arch. With loss of continuity of the pars interarticularis, “the intervertebral disc is not sufficiently strong to prevent displacement of the vertebrae.”
The forward displacement of spondylolisthesis is “most likely to be progressive during the rapid growth spurt of early adolescence.”
Spondylolytic spondylolisthesis “usually becomes manifest during childhood with the gradual onset of low back pain which is aggravated by standing, walking and running and relieved by lying down.”
“The associated clinical deformity, which is related to the degree of forward slip, is characterized by a ‘step’ in the lumbosacral region at the level of the spondylolisthesis and an increased lumbar lordosis above.”
- In 1987, Yochum and Rowe note:
The Eskimo infant is placed upright at an earlier age. This might account for the higher incidence of spondylolysis and spondylolisthesis in Eskimo populations.
- In 1988, Cailliet notes:
Seventy percent of spondylolysis and anterior spondylolisthesis occur at L5, 25% occur at L4, and 4% occur at higher levels. The low back is stiff with limited flexibility. “The patient frequently claims discomfort from lifting, excessive bending over, or from prolonged standing in a nonmoving manner.”
- In 1990, White and Panjabi note:
“In spondylolisthesis there is a defect in the pars interarticularis that is associated with anterior translation of the involved vertebrae in relation to the subjacent one.” “The theory that seems to have survived best at present is that of fatigue fracture.”
“The disease is thought to have an incidence of 1.95% in American blacks, 5.8% in American whites, and about 60% in American Eskimos.”
- In 2011, Cox notes:
“Isthmic spondylolisthesis is the most common type of spondylolisthesis, and it is caused by a defect in the ossification of the pars interarticularis.”
“It is no longer questioned that spondylolysis is a fracture that may or may not heal. These fractures are postulated to occur because of the assumption of the upright posture by the infant, allowing a fatigue type of fracture to occur when stress beyond the strength of bone occurs.”
“One reason that forward slippage occurs most often in children aged 5 to 7 years may be because of the increased activity or to increased sitting in the lordotic posture done by children. It is known that fracture never occurs in animals other than humans, and only humans have lordosis.”
“At the time of slippage, the disc must break down, allowing annular stretching and tearing.” “The disc, being a very pain-sensitive structure, certainly creates symptomatology as the slippage occurs.” “In adults, after the slippage occurs and the annular fibers heal, the pain lessens or disappears.”
•••••••••
Joe had some additional interesting and important examination findings:
- His low back range of motion was very limited, especially in flexion.
- His lumbosacral musculature was hypertonic with moderate spasm.
- There were no signs of motor or sensory radiculopathy or of myelopathy: deep tendon reflexes were normal bilaterally; there were no alterations in superficial sensation; lower extremity myotomal strength was normal and strong without fatigability in all tested muscles; Babinski’s test was normal; there were no reports of dysfunction in bowels, bladder or sexual function; Valsalva was normal; lumbar spine compression (Kemp’s) was normal. Although the recumbent straight-leg-raising test was negative for signs of compressive radiculopathy, Joe’s hamstring muscles were extremely tight; he could only raise his legs to about 30 degrees bilaterally as a consequence of hamstring tightness.
- While standing, a significant “shelf” was found above Joe’s L5 spinous process; it was so noticeable that a cup of liquid could be rested on the shelf without spilling.
•••••••••
Hamstring Tightness
As with Joe, hamstring tightness is a common and important finding in patients with clinically relevant spondylolysis and anterior spondylolisthesis. When the L5 vertebral body slides anterior and inferior, the L4 vertebral body travels forward with it. This elongates the distance the cauda equinal and sacral nerve roots must travel, as they must still traverse posteriorly to descend in the sacral canal. This effectively tethers or stretches these nerves. Several have postulated that this could account for the hamstring tightness:
- In 1980, Keim notes:
With increasing slippage, there is increasing stress on the sacral roots.
- In 1983, Salter notes:
“The hamstring muscles are tight with resulting limitation of straight leg raising.”
- In 1988 Cailliet notes:
“An interesting finding associated with spondylolisthesis but as yet unexplained is the presence of limited extensibility of the hamstring muscles. The hamstrings are ‘tight’ on straight leg raising but with negative dural signs.” “The cause of the tight hamstring muscle is conjectural and has been attributed to caudal equinal traction with irritation to the nerve roots descending to the hamstring muscles.”
- In 2011, Cox notes:
Clinical features include paravertebral muscle hypertrophy, increased lumbar lordosis, signs of slipping on inspection and/or palpation, hamstring muscle spasm, and pain during trunk flexion-extension tasks.
•••••••••
Step, Ledge, Shelf
As with Joe, an important examination finding of a clinically significant spondylolysis and anterior spondylolisthesis is the presence of a “step” or “ledge” or “shelf” on top of the L5 spinous process and the L4 spinous process. The inferior facet of L5 is still articulating with the superior facet of S1, meaning the L5 spinous process remains in its original position prior to the spondylolysis and anterior spondylolisthesis. However, the inferior facet of L4 slid anterior along with the body of L5 and the superior facet of L5. In fact, the entire spine above the L5 pars separation moves anteriorly, leaving behind the sacrum, the inferior facet of L5, and the L5 spinous process, effectively creating a step or ledge or shelf. Note:
- In 1971, Schmoral and Junghanns note:
“If the slippage has reached an advanced stage, then the physician can see and feel a step along the row of spinous processes since the spinous processes of the slipped vertebral body remains in its proper position and thus projects more posteriorly than the spinous processes situated above it.”
- In 1977, D’Ambrosia notes:
“The defect of a severe spondylolisthesis where the vertebral body slips forward on the one below, can be palpated as a step off in the lumbar spine.”
- In 1983, Salter notes:
“The associated clinical deformity, which is related to the degree of forward slip, is characterized by a ‘step’ in the lumbosacral region at the level of the spondylolisthesis and an increased lumbar lordosis above.”
- In 1988 Cailliet notes:
“The examination frequently reveals a palpable ‘ledge’ on passing the fingers down the lumbosacral spine.”
•••••••••
Pathology and Prognosis
The tissues affected by spondylolysis and anterior spondylolisthesis endure greater biomechanical stresses and associated spinal degenerative disease. These facts have long-term prognostic significance, as noted:
- In 1973, Farfan notes:
“It is clear that, with either a spondylolysis or a spondylolisthesis, the derangement of normal anatomic arrangements and loss of proper physiological function will lead to degenerative change in this joint.”
When the spondylolysis occurs early in childhood, the weak joint may heal and regain its normal strength. In such instances the next higher joint may be pushed into relative danger.”
- In 1977, Mcnab notes:
“Spondylolysis predisposes to premature disc degeneration in the subjacent disc and spondylolisthesis does not occur without disc degeneration. These degenerative changes may of themselves be painful, giving rise to local or referred pain in sciatic distribution without root irritation.”
- In 1983, Salter notes:
“Significant involvement of the nerve roots is not common in this type of spondylolisthesis although nerve root irritation may produce sciatica.”
- In 1995, Schneiderman and colleagues performed a histologic study on the pars defect tissue of six adult patients with symptomatic spondylolysis and spondylolisthesis to identify and characterize their neural elements.
“Histologic examination revealed extensive connective tissue scar formation throughout all specimens examined.”
“Free nerve endings believed to have nociceptive function were identified in all specimens.”
“The finding of neural elements, including free nerve endings within the pars defect tissue, suggests that the pars defect may be a source of back pain in some patients with symptomatic spondylolysis.”
“Our study identified within the pars defect neural elements capable of nociceptive function.”
“In conclusion, connective tissue and scar tissue harvested from the pars defect of symptomatic patients with spondylolysis contains a high density of neural tissue. Numerous elements consistent with nociceptive nerve endings have been identified. This finding suggests that the interposed tissue within the pars defect may be a source of back pain in some patients with symptomatic spondylolysis.”
- In 2011, Cox notes:
“Free nerve endings within the pars defect tissue can be a source of back pain in some patients with symptomatic spondylolysis.” “Pain in spondylolysis or spondylolisthesis might derive from the spondylolytic defect itself, probably from stretching of the local neural elements.”
“Forward slippage of the body will not occur without degenerative changes in the underlying disc (i.e., forward slippage is not possible without annular tearing or breakdown). The disc is not capable of withstanding the shearing stresses of the body above on the one below.”
•••••••••
Conservative Management
The pain of spondylolysis and spondylolisthesis is nearly always managed conservatively, which includes spinal manipulation and flexion distraction techniques (Cox). Reference examples include:
- In 1971, Schmoral and Junghanns note:
“Sports associated with considerable stress or with certain shearing motions involving the lumbosacral transition, such as weight-lifting, wrestling or judo, should be avoided. However, light sports activities and swimming are permitted.”
- In 1977, McNab notes:
“Spondylolysis predisposes to premature disc degeneration in the subjacent disc and spondylolisthesis does not occur without disc degeneration. These degenerative changes may of themselves be painful, giving rise to local or referred pain in sciatic distribution without root irritation.”
- In 1987, Yochum and Rowe note:
“A more conservative approach including chiropractic spinal manipulative therapy has been found beneficial in managing patients low back pain with the presence of spondylolysis or spondylolisthesis.”
- In 1988, Kirkaldy-Willis notes:
“Frequently, spondylolisthesis is complicated by a posterior joint syndrome one level above the lesion or by a sacroiliac syndrome. Thus, improvement in the patient’s symptoms results from the effect of manipulation on these other joints. In our experience, manipulation is a good first line of treatment in patients with spondylolisthesis. We have seen patients who did not benefit from [surgical] decompression and/or fusion but who were relieved of their back and leg pain by manipulation directed to the sacroiliac joint.”
•••••••••
Bracing and Surgical Consultation
An acute spondylolysis is a fracture. When history and imaging, including a bone scan, confirm an acute spondylolysis, the patient should undergo bracing immobilization (details beyond the scope of this paper).
In the majority of patients with spondylolysis and anterior spondylolisthesis, the lesion is stable. In top tier and professional athletes, the stability of their lesion causes little pain and essentially no dysfunction. However, when spondylolysis and spondylolisthesis become unstable, there often exists significant pain and neurological symptoms and signs, as well as functional deficits. Unstable patients should be referred for a surgical consultation.
Classically, stability status has been assessed with maximum flexion-neutral-maximum extension lateral radiography. However, Friberg described a more accurate assessment in 1987. The patient hangs from a bar with their hands/arms (bending their knees) while a lateral lumbar x-ray is exposed. In stable spondylolisthesis, the L5-S1 relationship will remain unchanged. If the sacrum slides under the L5 vertebral body while hanging, the patient has an unstable spondylolisthesis. This patient may require a surgical consultation and surgical stabilization.
REFERENCES
Cailliet R; Low Back Pain Syndrome; Fourth Edition; FA Davis; 1988.
Cox JM; Low Back Pain, Mechanism, Diagnosis, and Treatment; Seventh Edition; Wolters Kluwer/Lippincott Williams & Wilkins; 2011.
Cyriax J; The Slipped Disc, Causes, Prevention, and Treatment of a Universal Complaint; Second Edition, Grower Press, 1975.
D’Ambrosia RD; Musculoskeletal Disorders, Regional Examination and Differential Diagnosis; Lippincott, 1977.
Farfan HF; Mechanical Disorders of the Low Back; Lea & Febiger; 1973.
Finneson B; Low Back Pain; Second Edition; Lipponcott; 1980.
Friberg O; Lumbar instability: a dynamic approach by traction-compression radiography; Spine; March 1987; 12(2):119-29.
Kapandji IA; The Physiology of the Joints; Volume Three, The Trunk and the Vertebral Column; Churchill Livingstone; 1974.
Keim H; Low Back Pain, Clinical Symposium; Vol. 32; No. 6; CIBA; 1980.
Kirkaldy-Willis WH; Managing Low Back Pain; Second Edition; Churchill Livingstone; 1988.
Melamed A; SPONDYLOLYSIS AND SPONDYLOLISTHESIS ARE NOT CONGENITAL; Wisconsin Medical Journal; March 1965; 64:130-3.
McNab I; Backache; Williams & Wilkins, 1977.
Rosenberg NJ, Bargar WL, Friedman B; The incidence of spondylolysis and spondylolisthesis in non-ambulatory patients. Spine; 1981 Jan-Feb;6(1):35-8.
Salter RB; Textbook of Disorders and Injuries of the Musculoskeletal System; Second Edition; Williams and Wilkins; 1983.
Schmoral G, Junghanns H; Schmorl’s and Junghanns’ The Human Spine in Health and Disease; Grune & Stratton; 1971.
Schneiderman GA, McLain RF, Hambly MF, Nielsen SL; The pars defect as a pain source: A histologic study; Spine; August 15, 1995;20(16):1761-4
Wertzberger KL, Peterson HA; Acquired spondylolysis and spondylolisthesis in the young child; Spine (Phila Pa 1976). 1980 Sep-Oct;5(5):437-42.
White AA, Panjabi MM; Clinical Biomechanics of the Spine; Second Edition; Lippincott; 1990.
Yochum TR, Rowe LJ; Essentials of Skeletal Radiology; Williams & Wilkins; 1987.
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.