Integrating Connective Tissue and Nervous System Mechanisms
Medical Hypotheses
Volume 68, Issue 1, January 2007, Pages 74-80
Helene M. Langevin and Karen J. Sherman
The primary author is from the Department of Neurology, University of Vermont, College of Medicine.
FROM ABSTRACT
Although chronic low back pain (cLBP) is increasingly recognized as a complex syndrome with multifactorial etiology, the pathogenic mechanisms leading to the development of chronic pain in this condition remain poorly understood.
This article presents a new, testable pathophysiological model integrating connective tissue plasticity mechanisms with several well-developed areas of research on cLBP (pain psychology, postural control, neuroplasticity).
We hypothesize that pain-related fear leads to a cycle of decreased movement, connective tissue remodeling, inflammation, nervous system sensitization and further decreased mobility.
The integration of connective tissue and nervous system plasticity into the model of cLBP will potentially illuminate the mechanisms of a variety of treatments that may reverse these abnormalities by applying mechanical forces to soft tissues (e.g. physical therapy, massage, chiropractic manipulation, acupuncture), by changing specific movement patterns (e.g. movement therapies, yoga) or more generally by increasing activity levels (e.g. recreational exercise).
Non-invasive measures of connective tissue remodeling may eventually become important tools to evaluate and follow patients with cLBP in research and clinical practice.
THESE AUTHORS ALSO NOTE:
“Historically, mechanistic models for cLBP have tended to focus on musculoskeletal tissues, on the nervous system, or on behavior. In this paper, we propose a new, dynamic and integrative pathophysiological model for cLBP bringing together recent research on movement and neuroplasticity along with well-established connective tissue remodeling mechanisms.”
These authors propose that “plasticity in both connective tissue and nervous systems, linked to each other via changes in motor behavior, play a key role in the natural history of cLBP, as well as the response of cLBP to treatments and placebos.”
The “association between symptoms and imaging results (X-ray, CT, MRI) has been consistently weak, and up to 85% of patients with low back pain cannot be given a precise pathoanatomical diagnosis using these methods.”
“The generally poor predictive value of diagnostic imaging in cLBP, and the often disappointing effects of many ‘lesion-specific’ treatments such as intra-articular corticosteroid injections, has spurred research efforts toward ‘non-structural’ psychological and behavioral aspects of cLBP, and away from tissue pathology.”
“Rest may be initially important in the face of acute low back injury (e.g. disc herniation, muscle sprain), it is increasingly recognized that timely resumption of physical activity is critical to successful rehabilitation.”
“In addition to abnormal movement patterns, patients with cLBP have been shown to have generalized augmented pain sensitivity and cortical activation patterns suggesting abnormal central pain processing.”
“Ongoing pain is associated with widespread neuroplastic changes at multiple levels within the nervous system and including primary afferent neurons, spinal cord, brainstem, thalamus, limbic system and cortex.”
Neuroimaging has shown that there are distinct “brain networks” involved in acute vs. chronic pain. Chronic pain is specifically related to regions for cognition and emotions.
Chronic back pain results in neuronal or glial loss in the pre-frontal and thalamic gray matter.
Current models view chronic pain as a multisystem output, the “pain neuromatrix” includes both sensory and motor components.
“We hypothesize that connective tissue remodeling occurs in cLBP as a result of emotional, behavioral and motor dysfunction.”
“We further hypothesize that increased connective tissue stiffness due to fibrosis is an important link in the pathogenic mechanism leading to chronicity of pain, fear-avoidance and further movement impairment.”
[Very Important: The Fibrosis of Repair, Fibrotic Changes]
“Abnormal movement patterns can have important influences on the connective tissues that surround and infiltrate muscles.” [Very Important]
“A hallmark of connective tissue is its plasticity or ‘remodeling’ in response to varying levels of mechanical stress.”
“Both increased stress due to overuse, repetitive movement and/or hypermobility, and decreased stress due to immobilization or hypomobility can cause changes in connective tissue.”
“A chronic, local increase in stress can lead to microinjury and inflammation (overuse injury, cumulative trauma disorder).”
“A consistent absence of stress, on the other hand, leads to connective tissue atrophy, architectural disorganization, fibrosis, adhesions and contractures.”
“Fibrosis can be the direct result of hypomobility or the indirect result of hypermobility via injury and inflammation.” [Very Important]
During the early phase of immobilization, loss of muscle length is primarily due to shortening of muscle-associated connective tissue, which is later followed by actual shortening of muscle fibers.
Muscle connective tissue fibrosis promotes hypomobility. “Connective tissue fibrosis is detrimental, as it leads to increased tissue stiffness and further movement impairment.” [Important]
“Tissue microinjury, inflammation and fibrosis not only can change the biomechanics of soft tissue (e.g. increased stiffness) but also can profoundly alter the sensory input arising from the affected tissues.” [Very Important]
“Connective tissue is richly innervated with mechanosensory and nociceptive neurons.” [Very Important]
Activation of nociceptors can contribute to the development or worsening of fibrosis and inflammation, causing even more tissue stiffness and movement impairment. [Important]
In patients with cLBP, connective tissue fibrosis can occur in the lower back due to one or several of the following factors:
1) Decreased activity
2) Changes in muscle activation patterns causing muscle co-contraction, muscle spasm or tissue microtrauma
3) Neurally-mediated inflammation
Chronic low back pain may be caused by pathological connective tissue fibrosis, which causes adverse changes in movement. This is well documented in ligaments and joint capsules. [Very Important] This pathological connective tissue fibrosis is plastic and can therefore be remodeled. However, the remodeling must take place over time.
“In fibrosed connective tissue and muscle, blood and lymphatic flow may be chronically compromised by the disorganized tissue architecture and thus vulnerable to unusual muscle activity (e.g. beginning a new work activity or sport), or to conditions causing further decrease in perfusion such as prolonged sitting.”
Pain leads to reduced motion, and movement restriction increases fibrosis, “setting the patient up for more painful episodes.” [Very Important]
“In addition to its role in the pathological consequences of immobility and injury, the dynamic and potentially reversible nature of connective tissue plasticity may be key to the beneficial effects of widely used physical therapy techniques as well as ‘alternative’ treatments involving external application of mechanical forces (e.g. massage, chiropractic manipulation, acupuncture), changes in specific movement patterns (e.g. movement therapies, tai chi, yoga) or more general changes in activity levels (e.g. increased recreational exercise).”
“Manual or movement-based treatments have the advantage of not causing drug-induced side effects (e.g. gastritis, sedation),” but excessive motion may lead to inflammation.
A “carefully applied direct tissue stretch may be necessary in cases of long standing hypomobility with pronounced fibrosis and stiffness.”
[Very Important]
“The model presented in this paper predicts that beneficial connective tissue remodeling can result from a variety of therapeutic interventions.”
Connective tissue remodeling may be assessed with “non-invasive ultrasound based techniques such as ultrasound elastography.”
KEY POINTS FROM THIS ARTICLE:
1) In chronic low back pain, there is an integration between connective tissue fibrosis and the nervous system perception of pain.
2) Adverse connective tissue fibrosis can be remodeled by applying mechanical forces to soft tissues, including chiropractic spinal adjusting. [Note, chiropractic was included as the applying of a mechanical force to reverse adverse connective tissue fibrosis and its influence on the nervous system.]
3) The “association between symptoms and imaging results (X-ray, CT, MRI) has been consistently weak, and up to 85% of patients with low back pain cannot be given a precise pathoanatomical diagnosis using these methods.”
4) “Ongoing pain is associated with widespread neuroplastic changes at multiple levels within the nervous system and including primary afferent neurons, spinal cord, brainstem, thalamus, limbic system and cortex.”
5) Neuroimaging has shown that there are distinct “brain networks” involved in acute vs. chronic pain. Chronic pain is specifically related to regions for cognition and emotions.
6) Chronic back pain results in neuronal or glial loss in the pre-frontal and thalamic gray matter. [Brain atrophy]
7) “Increased connective tissue stiffness due to fibrosis is an important link in the pathogenic mechanism leading to chronicity of pain.”
8) “Abnormal movement patterns can have important influences on the connective tissues that surround and infiltrate muscles.” [Very important because the subluxation complex includes abnormal movement patterns.]
9) “A hallmark of connective tissue is its plasticity or ‘remodeling’ in response to varying levels of mechanical stress.” [This is important because it implies that spinal adjusting can initiate remodeling of abnormal connective tissues.]
10) “Both increased stress due to overuse, repetitive movement and/or hypermobility, and decreased stress due to immobilization or hypomobility can cause changes in connective tissue.”
[Both increased and decreased motion are deleterious.]
11) A chronic local increase in stress leads to micro-injury and inflammation.
[Subluxation can cause micro-injury and inflammation.]
12) “A consistent absence of stress leads to connective tissue atrophy, architectural disorganization, fibrosis, adhesions and contractures.” [Fibrosis]
13) “Fibrosis can be the direct result of hypomobility or the indirect result of hypermobility via injury and inflammation.” [Very Important]
14) During the early phase of immobilization, loss of muscle length is primarily due to shortening of muscle-associated connective tissue, which is later followed by actual shortening of muscle fibers.
15) Muscle connective tissue fibrosis promotes hypomobility. “Connective tissue fibrosis is detrimental, as it leads to increased tissue stiffness and further movement impairment.” [Important, Fibrosis]
16) “Tissue microinjury, inflammation and fibrosis not only can change the biomechanics of soft tissue (e.g. increased stiffness) but also can profoundly alter the sensory input arising from the affected tissues.” [Very Important: many contend that the tissue changes associated with the subluxation alter the afferent input into the CNS, which is the nerve interference of the subluxation.]
17) “Connective tissue is richly innervated with mechanosensory and nociceptive neurons.” [Very Important]
18) Activation of nociceptors can contribute to the development or worsening of fibrosis and inflammation, causing even more tissue stiffness and movement impairment. [Important]
19) Chronic low back pain may be caused by pathological connective tissue fibrosis, which causes adverse changes in movement. This is well documented in ligaments and joint capsules. [Very Important] This pathological connective tissue fibrosis is plastic and can therefore be remodeled. However, the remodeling must take place over time.
20) “In fibrosed connective tissue and muscle, blood and lymphatic flow may be chronically compromised by the disorganized tissue architecture and thus vulnerable to unusual muscle activity (e.g. beginning a new work activity or sport), or to conditions causing further decrease in perfusion such as prolonged sitting.”
21) Pain leads to reduced motion, and movement restriction increases fibrosis, “setting the patient up for more painful episodes.” [Very Important, Fibrosis]
22) “In addition to its role in the pathological consequences of immobility and injury, the dynamic and potentially reversible nature of connective tissue plasticity may be key to the beneficial effects of widely used physical therapy techniques as well as ‘alternative’ treatments involving external application of mechanical forces (e.g. massage, chiropractic manipulation, acupuncture), changes in specific movement patterns (e.g. movement therapies, tai chi, yoga) or more general changes in activity levels (e.g. increased recreational exercise).”
23) “Manual or movement-based treatments have the advantage of not causing drug-induced side effects (e.g. gastritis, sedation),” but excessive motion may lead to inflammation.
24) A “carefully applied direct tissue stretch may be necessary in cases of long standing hypomobility with pronounced fibrosis and stiffness.”
[Very Important, as a chiropractic adjustment may be considered to be a “carefully applied direct tissue stretch.”]
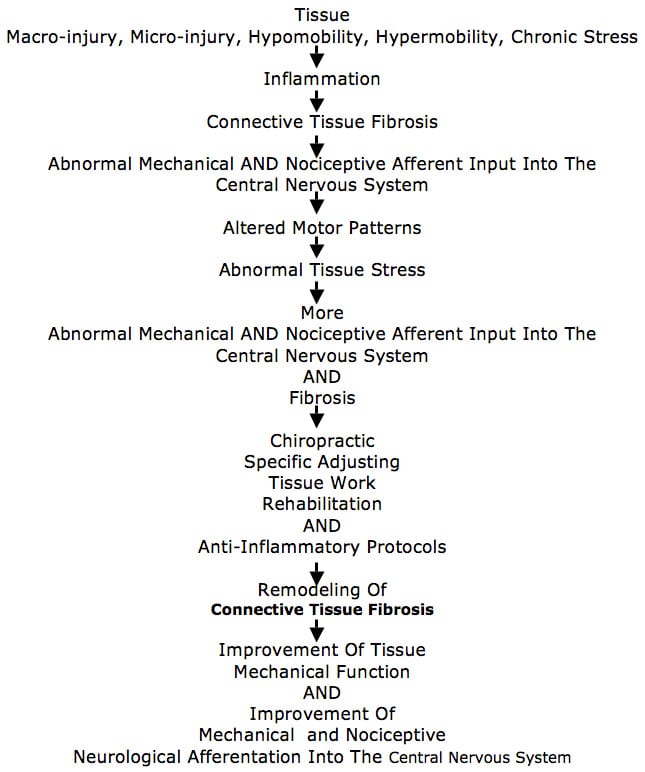
A Model Based Upon This Article
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.

