British Medical Journal
March 10, 2007;334:527-531
Allan I Binder, consultant rheumatologist
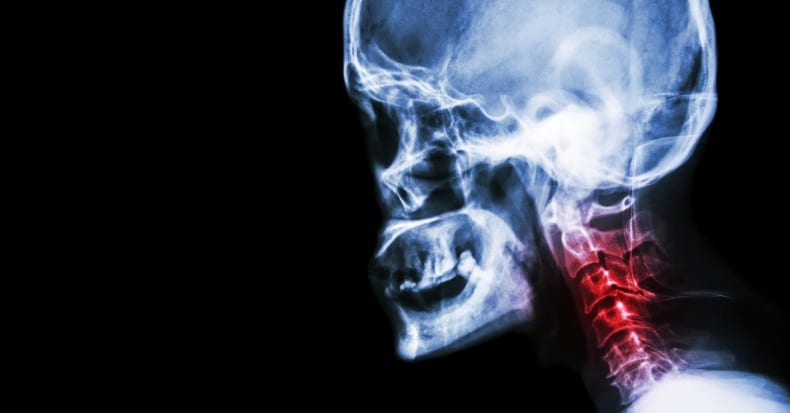
Presenting Features of Cervical Spondylosis
SYMPTOMS
* Cervical pain aggravated by movement
* Referred pain (occiput, between the shoulder blades, upper limbs)
* Retro-orbital or temporal pain (from C1 to C2)
* Cervical stiffness—reversible or irreversible
* Vague numbness, tingling, or weakness in upper limbs
* Dizziness or vertigo
* Poor balance
* Rarely: syncope, migraine, “pseudo-angina”
SIGNS
* Poorly localized tenderness
* Limited range of cervical movement
* Minor neurological changes like inverted supinator jerks (unless complicated by myelopathy or radiculopathy)
Differential Diagnosis of Cervical Spondylosis
* Other non-specific neck pain lesions—acute neck strain, postural neck ache, or whiplash
* Fibromyalgia
* Mechanical lesions—disc prolapse or diffuse idiopathic skeletal hyperostosis
* Inflammatory disease—rheumatoid arthritis, ankylosing spondylitis, or polymyalgia rheumatica
* Metabolic diseases—Paget’s disease, osteoporosis, gout, or pseudo-gout
* Infections—osteomyelitis or tuberculosis
* Malignancy—primary tumors, secondary deposits, or myeloma
RED FLAG Features and the Conditions they May Suggest
Malignancy, infection, or inflammation
* Fever, night sweats
* Unexpected weight loss
* History of inflammatory arthritis, malignancy, infection, tuberculosis, HIV infection, drug dependency, or immunosuppression
* Excruciating pain
* Intractable night pain
* Cervical lymphadenopathy
* Exquisite tenderness over a vertebral body
Myelopathy
* Gait disturbance or clumsy hands, or both
* Objective neurological deficit—upper motor neuron signs in the legs and lower motor neuron signs in the arms
* Sudden onset in a young patient suggests disc prolapse
Other
* History of severe osteoporosis
* History of neck surgery
* Drop attacks, especially when moving the neck, suggest vascular disease
SUMMARY POINTS FROM AUTHOR:
The diagnosis of cervical spondylosis is usually based on clinical symptoms.
Patients need detailed neurological assessment of upper and lower limbs, as cervical degeneration is often asymptomatic, but can lead to pain, myelopathy, or radiculopathy.
“Red flag” symptoms identify the small number of patients who need magnetic resonance imaging, blood tests, and other investigations.
The best treatments are exercise, manipulation, and mobilization, or combinations thereof.
Radiculopathy has a good prognosis and may respond to conservative measures.
Results of neck surgery for myelopathy or intractable pain are often disappointing.
FROM ABSTRACT:
Most patients who present with neck pain have “non-specific (simple) neck pain,” where symptoms have a postural or mechanical basis.
Etiological factors are poorly understood and are usually multifactorial, including poor posture, anxiety, depression, neck strain, and sporting or occupational activities.
Neck pain after whiplash injury also fits into this category, provided no bony injury or neurological deficit is present.
When mechanical factors are prominent, the condition is often referred to as “cervical spondylosis,” although the term is often applied to all non-specific neck pain.
Mechanical and degenerative factors are more likely to be present in chronic neck pain.
In cervical spondylosis, degenerative changes start in the intervertebral discs with osteophyte formation and involvement of adjacent soft tissue structures.
Many people over 30 show similar abnormalities on plain radiographs of the cervical spine, so the boundary between normal ageing and disease is difficult to define.
Even severe degenerative changes are often asymptomatic, but can lead to neck pain, stiffness, or neurological complications.
THIS AUTHOR ALSO NOTES:
66% of the population will have neck pain at some time in their lives.
The prevalence of neck pain is highest in middle age.
25% of women have current neck pain.
20% of men have current neck pain.
34% of the population had experienced neck pain in the previous year.
“After back pain, neck pain is the most frequent musculoskeletal cause of consultation in primary care worldwide.”
“In the UK about 15% of hospital based physiotherapy and in Canada 30% of chiropractic referrals are for neck pain.”
Neck pain places a heavy burden on individuals, employers, and healthcare services.
10% of those who develop acute neck pain will develop chronic neck pain.
Neck related disorders account for as much time off work as low back pain.
Neck pain causes severe disability in 5% of affected people.
In patients with cervical spondylosis, “neurological change should always be sought in the upper and lower limbs, but objective changes occur only when spondylosis is complicated by myelopathy or radiculopathy, or when unrelated causes like disc prolapse, thoracic outlet obstruction, brachial plexus disease, malignancy, or primary neurological disease are present.”
Plain radiographs of the cervical spine may show features of degenerative disease, but are also “found in asymptomatic people and correlate poorly with clinical symptoms.”
“Magnetic resonance imaging of the cervical spine is the investigation of choice if more serious pathology is suspected, as it gives detailed information about the spinal cord, bones, discs, and soft tissue structures.”
“Cervical spondylosis can be complicated by myelopathy or radiculopathy, although cervical disc prolapse, plexopathy, motor neuron disease” cause similar symptoms.
“Neurological complications can occur in established cervical spondylosis or can be the presenting feature of the disease.”
“Myelopathy causes clumsiness of the hands or gait disturbance, or both, as a result of sensory ataxia or spastic paraparesis of the lower limbs, with bladder dysfunction being a late symptom.”
Examination of the upper limbs of patients with spondylosis may show:
1) Increased muscle tone, with a pronator “catch” (C6/C7).
2) Increased tone in the finger flexors (C8).
3) “Wasting and fasciculation of biceps (C5/C6) or triceps (C7) are occasional findings.”
4) “The lower limbs usually show an increase in tone with spasticity, but little true weakness.”
5) “Tendon reflexes are characteristic, with reduced or even inverted biceps or supinator jerks (finger flexion instead of the normal biceps or supinator jerk), and an increase in triceps jerks, finger jerks, and all lower limb reflexes, with upgoing plantar responses.”
6) “A positive Hoffman’s sign (flexion of the terminal phalanx of the thumb and second and third phalanges of the other fingers when one of the middle fingertips is flicked) and ankle clonus are also common findings.”
7) Sensory changes tend to affect vibration and joint position sense in the hands more than the feet.
Radiculopathy (nerve root compression) due to cervical spondylosis usually occurs at the C5 to C7 levels.
In classical upper limb radiculopathy, sensory symptoms (shooting pains, numbness, hyperaesthesia) are more common than weakness. [Important]
Reflexes are usually diminished at the appropriate level (biceps (C5/6), supinator (C5/6), or triceps (C7)).
Most mechanical neck pain will respond to conservative measures.
“Stress management and postural advice on daily activities, work, and hobbies may be useful in some patients.”
“Patients should be advised to use only one pillow at night.”
“Analgesics and anti-inflammatory agents are widely used, despite the lack of evidence that they work.”
In the treatment of acute neck pain, “no evidence exists for the efficacy of non-steroidal anti-inflammatory agents or analgesics.”
“Studies of the early treatment of whiplash provide moderate evidence that early mobilisation physiotherapy and advice to “act as usual” are more effective than immobilisation and less active treatments in speeding up recovery and reducing chronic disability.”
“Randomised controlled trials included in systematic reviews of manual treatments (mobilisation physiotherapy or manipulation) provide limited evidence that mobilisation physiotherapy and manipulation are more effective for chronic neck pain than less active treatments (drug treatment, education, counseling).”
Mobilisation, manipulation, and exercise are all effective in treating neck pain.
“Most patients with neurological abnormality will need magnetic resonance imaging of the cervical spine at an early stage, particularly if they have progressive myelopathy, radiculopathy, or intractable pain.”
“Neurosurgical intervention also needs to be considered, but the outcome of decompressive surgery is often disappointing, especially for myelopathy complicating cervical spondylosis.”
“While progression of the neurological deficit may be slowed by surgery, lost function may not recover or symptoms may progress at a later date. Poor outcome after surgery may reflect irreversible damage to the cervical cord or compromise to the vascular supply to the cord.”
“Radiculopathy usually has a favourable outcome, so conservative treatments are gaining popularity.”
“Epidural injection in the cervical region is more invasive than in the lumbar region, and it should be considered in patients with severe intractable pain or radiculopathy only if surgical intervention is not an option.”
“Recently, better quality randomised controlled trials have suggested that exercise, mobilisation physiotherapy, and manipulation are more effective than less active treatments.”
“One high quality study suggested further advantages to combining exercise with mobilisation or manipulation; this approach has been advocated by a Cochrane review group and warrants further study.”
KEY POINTS FROM THIS AUTHOR
1) The symptoms of cervical spondylosis include neck pain aggravated by movement, referred pain to the occiput – between the shoulder blades – upper limbs, referred pain to the retro-orbital or temporal region from C1 to C2, neck stiffness, vague numbness – tingling or weakness in upper limbs, dizziness or vertigo, poor balance, and rarely syncope – migraine or “pseudo-angina”.
2) Cervical degeneration is often asymptomatic, but can lead to pain, myelopathy, or radiculopathy.
3) The best treatments for cervical spondylosis are exercise, manipulation, and mobilization, or combinations thereof.
4) Cervical radiculopathy has a good prognosis and usually responds well to conservative measures.
5) The results of neck surgery for myelopathy or intractable pain are often disappointing.
6) Most neck pain has a postural or mechanical basis.
7) Severe cervical degenerative changes are often asymptomatic but can lead to neck pain, stiffness, or neurological complications.
8) 66% of the population will have neck pain at some time in their lives.
9) The prevalence of neck pain is highest in middle age.
10) 25% of women have current neck pain.
11) 20% of men have current neck pain.
12) 34% of the population had experienced neck pain in the previous year.
13) “After back pain, neck pain is the most frequent musculoskeletal cause of consultation in primary care worldwide.”
14) About 30% of chiropractic referrals are for neck pain.
15) 10% of those who develop acute neck pain will develop chronic neck pain.
16) Neck related disorders account for as much time off work as low back pain.
17) Neck pain causes severe disability in 5% of affected people.
18) Magnetic resonance imaging of the cervical spine is the investigation of choice for cervical spondylosis, “as it gives detailed information about the spinal cord, bones, discs, and soft tissue structures.”
19) Cervical “myelopathy causes clumsiness of the hands or gait disturbance, or both, as a result of sensory ataxia or spastic paraparesis of the lower limbs, with bladder dysfunction being a late symptom.”
20) Most mechanical neck pain will respond to conservative measures.
21) In the treatment of acute neck pain, “no evidence exists for the efficacy of non-steroidal anti-inflammatory agents or analgesics.”
22) “Studies of the early treatment of whiplash provide moderate evidence that early mobilisation physiotherapy and advice to “act as usual” are more effective than immobilisation and less active treatments in speeding up recovery and reducing chronic disability.”
23) “Randomised controlled trials included in systematic reviews of manual treatments (mobilisation physiotherapy or manipulation) provide limited evidence that mobilization, physiotherapy and manipulation are more effective for chronic neck pain than less active treatments (drug treatment, education, counseling).”
24) Mobilisation, manipulation, and exercise are all effective in treating neck pain.
25) In the treatment of neck pain and cervical spondylosis, “better quality randomized controlled trials have suggested that exercise, mobilization physiotherapy, and manipulation are more effective than less active treatments.”
26) “One high quality study suggested further advantages to combining exercise with mobilisation or manipulation; this approach has been advocated by a Cochrane review group and warrants further study.”
Thousands of Doctors of Chiropractic across the United States and Canada have taken "The ChiroTrust Pledge":
“To the best of my ability, I agree to
provide my patients convenient, affordable,
and mainstream Chiropractic care.
I will not use unnecessary long-term
treatment plans and/or therapies.”
To locate a Doctor of Chiropractic who has taken The ChiroTrust Pledge, google "The ChiroTrust Pledge" and the name of a town in quotes.
(example: "ChiroTrust Pledge" "Olympia, WA")
Content Courtesy of Chiro-Trust.org. All Rights Reserved.